Graduate/PG Certificate Enhanced Evidence Based Practice (Children, Young People and Families)
Competencies
The University of Exeter CYP IAPT EEBP Programme has been designed in line with the generic CAMHS competency Framework (Roth and Pilling, 2011; see page 18) and the CYP IAPT national curriculum. The CBT Competencies Framework will also be drawn upon where appropriate (Roth & Pilling, 2007; see page 18) in addition to Reach Out materials for low intensity working.
For further Information on CAMHS Competencies, please visit: http://www.ucl.ac.uk/clinical-psychology/CORE/child-adolescent-competences/CAMHS%20Competences%20Framework_V1%20(2).pdf
For further information on CBT Competences, please visit: www.ucl.ac.uk/clinical-psychology/CORE/CBT_Framework.htm
We are very excited to bring you the CYP Improving Access to Psychological Therapies (IAPT) G/PG Certificate in Enhanced Evidence Based Practice. This training complements our already highly successful and expanding portfolio of IAPT programmes and contributes to our wider clinical training portfolio which includes the Doctorate in Clinical Psychology and the MSc Psychological Therapies. We also have a firm commitment to evidence based clinical practice and as such we endeavour to ensure all of our training programmes are firmly embedded within current research. This commitment is in no small way aided through the Mood Disorders Unit which is involved in undertaking clinical research which has national and international significance.
These are exciting and challenging times for us all. The team of highly experienced clinical trainers will endeavour to deliver the highest quality IAPT training to support you in transforming mental health services for children, young people and families.
It is likely that you will find the training intensive and challenging, but hopefully enjoyable and especially practice enhancing.
Professor Eugene Mullan, Director of Clinical Professional Training
Welcome to the University of Exeter’s Graduate/Postgraduate Certificate programme in Enhanced Evidence Based Practice (EEBP) for Children and Young People. This programme is part of the national Children and Young People’s Improving Access to Psychological Therapies (CYP IAPT) initiative.
The overall aims of the CYP IAPT Programme are to transform mental health services for young people and their families/carers; to maximise their effectiveness and efficiency and thus improve access to evidence-based and outcome-monitored interventions.
The EEBP programme complements the existing CYP IAPT programme in specialist psychological therapies (CBT, Systemic Family Practice, and Parenting Training for Conduct Problems.) It focuses on enhancing skills in assessment; delivering brief, low intensity, evidence based interventions and in the core competencies required to work with children and young people. The programme is heavily rooted within the development of clinical skills associated with a patient-centred approach and on the skills required to support brief evidence based therapies with CYP who are experiencing mild difficulties with anxiety and depression. The continued development of these skills is embedded within a strong focus on practice-based supervision, which is a fundamental component of the training. As such your training should not just be seen as being the time you spend being taught within the University, but full time, based also around your clinical work undertaken within your work setting supplemented by your practice based supervision.
Successful completion of clinical and academic assignments and appropriate participation in tutorials and workshops (both within the University and within your workplace) will lead to the awarding of a G/ PG Certificate. We hope that you will be able to act as ‘product champions’ for brief, low intensity, evidence based interventions and to be available as teachers and consultants in the various CYP IAPT settings in which you work. A major contributing resource to the programme is the knowledge and experiences that you as programme members bring. We intend to draw upon and honour this knowledge and experience in order to develop clinical skills and increase awareness and theoretical understanding. It is important, however, that understanding and use of theory is integrated with clinical application in a rigorous and constructively critical manner.
We hope you enjoy the training and look forward to meeting you over the coming months.
Dr Catherine Gallop, Director of CYP IAPT Programmes
| Name | Title | |
|---|---|---|
| Professor Eugene Mullan | Director of Clinical Professional Training | |
| Professor Catherine Gallop | Director of CEDAR PGT Programmes | c.a.gallop@exeter.ac.uk |
| Dr Rob Kidney | Programme Lead | R.J.Kidney2@exeter.ac.uk |
| Dr Fin Williams | Academic Lead | F.Williams@exeter.ac.uk |
| Kat Sexton | EEBP Tutor | K.Sexton@exeter.ac.uk |
| Beth MacLachlan | Programme Administrator | B.MacLachlan@exeter.ac.uk |
In this programme we aim to help you develop your practice in brief, low intensity, evidence-based psychological intervention for children, young people and their families. You will develop the knowledge and competencies required to be an effective practitioner, as determined by the relevant national curriculum for the CYP IAPT EEBP Programme. Specifically, we will help you develop skills in assessment; delivering brief, low intensity, evidence based interventions and in the core competencies required to work with children and young people.
We aim to provide you with a high quality and stimulating learning experience in a supportive environment that is enriched by an internationally recognised research environment, nationally recognised innovative clinical teaching approaches and current clinical practice.
The programme aims to ensure that all graduates meet recognised minimum clinical competence in their practice, using brief, low intensity evidence-based psychological interventions for children, young people and their families.
Programme Aims
The overall aim of the programme is to provide an introduction to the theory and practice of evidence based practice, specifically low intensity Cognitive Behavioural Therapy (CBT). The programme will aim to provide an equal balance between theoretical knowledge of CBT and opportunity to integrate theory to clinical practice.
Specific programme aims are:
- To familiarise students with the core principles of CYP IAPT programmes, and apply these to their work with children, young people and families
- To develop appropriate competence in engaging the child, young person and their family and in specific interviewing skills
- To enable students to carry out a comprehensive cognitive behavioural assessment, incorporating assessment of risk and consideration of the child’s development and mental health diagnosis
- To develop an awareness and knowledge of cognitive behavioural models of specific disorders (anxiety and depression)
- To encourage the student to seek out and utilise clinical supervision and to base their clinical interventions on evidence based practice
- To enable students to carry out specific, brief evidence based interventions for anxiety disorders and depression in children and young people
- To develop appropriate competence in working with parents
- To enable students to function independently and reflectively as a learner and practitioner.
Learning methods
The EEBP curriculum uses a range of teaching methods including e-learning, service based learning days via group PBL and learning sets and supervised clinical practice in the workplace and workshops, skills practice and classroom learning at university. It focuses on the development of core skills and is assessed largely through the assessment of direct clinical work. The clinical skills taught are suitable for delivery in a range of settings including the voluntary sector, social and educational settings and the NHS.
Learning outcomes
At the end of the EEBP programme, successful students will:
- Understand the core components of a successful CYP IAPT programme
- Demonstrate how these core components are incorporated into their work with children, young people and their families
- Conduct a comprehensive assessment of a child/young person/their family within an evidence based framework, also considering elements of risk, development, and mental health diagnosis
- Carry out brief evidence based interventions for anxiety disorders and depression with children, young people and their families
- Use clinical supervision and demonstrate evidence of self-reflection in relation to their clinical work.
Programme Structure
There are three modules at Grad Cert level and three at PG Cert level within the EEBP Programme (All modules total up to 60 credits):
1. Core Skills;
2. Engagement and Assessment Skills; and
3. Evidence Based Interventions.
Modules
|
Code |
Title |
Credits |
| PYC3001/
PYCM007 |
Core Skills for Working with Young People with Mental Health Problems and Their Families | 15 |
| PYC3002/
PYCM008 |
Engagement and Assessment Skills with Children, Young People and Families | 15 |
| PYC3003/
PYCM009 |
Evidence Based Interventions with Children, Young People and Families | 30 |
Module Aims
| Code | Title and Aims |
|
PYC3001/ PYCM007 |
In this module you will develop your knowledge in the core principles of CYP IAPT and you will become skilled in enhancing your work with children, young people and their families/parents. This module underpins module 2 (assessment) and 3 (interventions). |
|
PYC3002/ PYCM008 |
In this module you will develop your core engagement skills and become skilled in using a range of methods to conduct comprehensive, structured assessments with children, adolescents and their families/parents. You will develop the knowledge and skills to develop a shared understanding about the child’s/young person’s difficulties. |
|
PYC3003/ PYCM009 |
In this module you will develop the essential skills necessary to provide an evidence based intervention based on the child’s/young person’s presentation. You will develop the core competencies to become an effective practitioner delivering brief, low intensity, evidence based interventions. |
Module Descriptors
Specifications for each module detailing Aims, Intended Learning Outcomes, Hours of Study, Details of Learning/Teaching activity, Assessments, Learning resources and Module details including Credit value.
Throughout this programme there is an emphasis upon you taking responsibility for some of your own education as independent learners. Your University teaching is timetabled, however study above and beyond these days, as with all University programmes, will be expected.
Work-base directed learning:
In order to support your University teaching and independent study, there are also workplace directed learning days in which you will undertake activities given to you that build on the University teaching sessions. You are not in University for these days as the tasks you carry out are most suited to you undertaking work with other trainees and also directed learning/skills practice rather than being in a classroom setting. These days are timetabled sessions and mandatory parts of your learning. Therefore they should be considered equally as important as the days that you attend the University. The days are full days equivalent to the hours you would be in University if you were undertaking these tasks and are part of your University requirements to pass the award. Carrying out these tasks helps to consolidate, refine and deepen your knowledge as well as helping you practice your clinical skills to work towards being competent in the clinical methods.
The days are full days equivalent to the hours you would be in University if you were undertaking these tasks and are part of your University requirements to pass the award. The content of these sessions is specified within the teaching timetable. You will be required to submit evidence that you have worked through the content of these days to the University, and you will be required to complete a self-reflection handout on these days.
These days count towards your minimum attendance requirement of the programme. We have a responsibility to ensure that you are able to undertake these days; so please do speak to us if there are any difficulties in you being given this time as it is essential for you to have the full training. All services are being reminded of the importance of these days to your training.
Problem-based learning:
Problem-based learning (PBL) is consistent with the adult learning model that we seek to promote. Working on problems collaboratively in a small group environment draws on a range of skills and abilities that are often unfamiliar to students. PBL has been used extensively in many areas of higher education since the 1970s, and research has found it to have a number of educational advantages.
Broadly speaking PBL is characterised by the use of problem scenarios, often based around clinical material. This provides a context to learn problem-solving skills, and in doing so, acquire knowledge. PBL will be used by the EEBP programme largely for the work-base directed learning days, when students will work within small groups in their service setting/geographical area.
PBL is characterised by the following:
- It uses stimulus material (in this instance clinical cases or referrals for psychological input) to engage students in considering the problem in the same context as ‘real life’
- Information is not given on how to tackle the problem
- Information is given to help clarify the problem and how it might be dealt with
- Students work co-operatively in small groups with access to a member of staff who facilitates the process
- Learning that has occurred is summarised and integrated into the students’ existing knowledge and skills
- Work is carried out intensively into one problem over a period of time
Within the curriculum, PBL will not be used to replace, but to complement and facilitate learning from the more traditional University teaching sessions. The clinical problems will cover a range of learning areas taken from the CYP IAOT area of work and with more general learning objectives, all relating to the core competencies needed for practice. They may be based around clinical casework or involve service issues.
Students will be encouraged to nominate a chair and scribe for these meetings who will record actions to be taken by group members. Students will then work independently, contributing to the group’s goals of finding solutions to the problems raised within the clinical case. Students will be expected to draw on a wide range of resources, including for example their own past experience, the library, and the internet, in the completion of these tasks.
Developing and enhancing clinical competence through self-practice/self-reflection (SPSR):
A major focus of the programme is placed upon the development of competence across a range of brief, low intensity interventions. A major focus of your time within the university taught days, the work-base directed learning days and your study days is on your own practice and the rehearsal of the interventions presented during the programme. To help structure and formalise this component of the programme (in particular the work-base directed learning days) the Self-Practice/Self-Reflection (SP/SR) model of supervision (Bennett-Levy et al., 2001; Farrand et al., 2010) will be adopted.
This model of supervision requires you to initially undertake the brief, low Intensity interventions presented during the programme on yourself, and then reflect upon your use. Rather than provide areas for you to focus your reflections around for each intervention which can be unnecessarily limiting, you are encouraged to provide widespread reflections on anything that arises concerning your own self-practice.
Teaching Days 2016
Term 1
Week 1 - Friday 5th February (University Teaching Day)
Week 2 - Thursday 11th February to Friday 12th February*
HALF TERM: 15th February - 19th February
Week 3 - Friday 26th February (University Teaching Day)
Week 4 - Friday 4th March (University Teaching Day)
Week 5 - Friday 11th March (University Teaching Day)
Week 6 - Friday 18th March*
EASTER TERM: 28th March - 23rd April
Term 2
Week 1 - Friday 29th April (University Teaching Day)
Week 2 - Friday 6th May*
Week 3 - Friday 13th May*
Week 4 - Friday 20th May (University Teaching Day)
HALF TERM: 23rd May - 27th May
Week 5 - Friday 3rd June (University Teaching Day)
Week 6 - Friday 10th June (University Teaching Day)
Week 7 - Friday 17th June*
Week 8 - NO TEACHING
Week 9 - Friday 1st July (University Teaching Day)
Week 10 Friday 8th July (University Teaching Day)
SUMMER BREAK: 11th July - 5th September
Term 3
Week 1 - Friday 9th September (University Teaching Day)
Week 2 - Friday 16th September*
Week 3 - NO TEACHING
Week 4 - NO TEACHING
Week 5 - Friday 7th October*
Week 6 - Friday 14th October (University Teaching Day)
Week 7 - NO TEACHING
HALF TERM: 24th October - 28th October
Week 8 - Friday 4th November (University Teaching Day)
Week 9 - Friday 11th November*
Week 10 - NO TEACHING
Week 11 - Friday 25th November*
Week 12 - Friday 2nd December (University Teaching Day)
END OF COURSE
*Sessions held offsite for Workplace Directed Learning.
Please note: the course is not formally completed until the successful submission of all examined work and the diploma is not awarded until the Award Board has met.
Office Hours
Contact the CYpIAPT Administrator (Beth MacLachlan) for helpwith any administrative queries.
You can contact the EEBpProgramme team by email with any programme queries you may have. They will be happy to arrange an individual time to meet if needed.
Feedback
Student must complete electronic feedback on ELE for each of their teaching sessions. These are per topic, rather than per day of teaching.
Feedback consists of a brief questionnaire and should easily be completed within 1-3 minutes. You will also need to evidence that you have completed feedback as part of your Clinical Portfolio assessment.
Feedback provides an opportunity for students to give their opinions and thoughts on teaching sessions and allows the CYpIAPT team to implement new suggestions and changes for future cohorts.
Location of Teaching
All University Teaching will take place in the Washington Singer Building or Reed Hall, University of Exeter.
Work-Based Directed Learning will be confirmed with you directly and will take place in groups within a service in your locality.
Work-Based Supervision will be confirmed with you directly and will take place in groups within a service in your locality. This will take place on a Monday, Tuesday or Wednesday).
The Structure and Timings of the days:
University teaching days: Thursdays/Fridays
9.45am – 4.45pm - Large group workshops
12.45pm–1.45pm - Lunch
Work-base directed learning days: Thursdays/Fridays
9.45 - 4.45
Study Time
Trainees are required by National Guidance to have a minimum of 28 days study time in addition to taught hours. We have timetabled in 6 days study time during half terms. It is recommended that the remaining 22 days are spread throughout the year, either as a half day each week or an arrangement that works best for the programme member and their employer.
Individual 1:1 Tutorials
- 1 x 20 minutes tutorial per term
Purpose
- Opportunity to review and reflect on your development and the course
- Opportunity to give and receive feedback on assessed work.
- Opportunity to give and receive feedback on the course.
- To review your clinical portfolio.
- A safe environment for addressing personal development.
NB: If trainees have any concerns or issues that may be impacting on their ability to participate fully in the training or causing them any distress or concern, trainees are strongly encouraged to notify either their tutor or any member of the course team as soon as possible, rather than wait for their 1:1 tutorial.
Preparation
Trainees are required to bring up to date forms each term for their individual tutorials, to include where appropriate:
- Clinical Log
- Supervision Log
- Teaching Log
- Practice Outcomes Assessment
Forms
Assessment Hand-In Procedure (EEBP)
Practitioners Assessment Summary
|
Assessment Element |
% of Marks |
Deadline | Marks Returned |
|---|---|---|---|
|
PYC3001/PSYM007 Core Skills |
|||
|
SUMMATIVE Short Answer Question Examination |
100% |
29/04/2016 | 20/05/2016 |
|
PYC3002/PSYM008 Engagement and Assessment |
|||
|
FORMATIVE Clinical skills competency assessment of an assessment session |
N/A
|
20/05/2016 |
20/06/2016 |
|
FORMATIVE Reflective commentary of an assessment session |
|||
|
SUMMATIVE Clinical skills competency assessment of an assessment session |
75% | 09/09/2016 | 07/10/2016 |
| SUMMATIVE Reflective commentary related to assessment session | 25% | ||
| PYC3003/PSYM009 Evidence-based Intervention | |||
|
FORMATIVE Clinical skills competency assessment of an intervention session |
N/A |
08/07/2016 |
05/08/2016 |
| FORMATIVE Reflective commentary of intervention session | |||
| SUMMATIVE Short Answer examination | 25% | 14/10/2016 | 04/11/2016 |
| SUMMATIVE Clinical skills competency assessment of an intervention session | 50% | 04/11/2016 | 02/12/2016 |
| SUMMATIVE Reflective commentary related to intervention session | 25% | ||
| PYC3001/PYC3002/PYC3003 All Modules | |||
| SUMMATIVE Clinical Portfolio | P/F | 02/12/2016 | 13/01/2017 |
| SUMMATIVE Supervisor Practice Outcomes Assessment | P/F | ||
The following are the methods by which your knowledge, clinical and reflective practice will be assessed:
- Short answer question examination
-
Clinical skills competency assessment (video recording)
-
Reflective commentary
-
Supervisor Practice Outcomes Assessment
- Clinical Portfolio
Workplace Service Leads and workplace Supervisors will be routinely informed of trainees' marks on their academic assignments (e.g. essays, case reports) and clinical assignments (e.g. competency CTS-R assessments). Workplace Service Leads and Supervisors are invited to make contact with the Academic Lead and Clinical Lead should any concerns about a trainee's development arise throughout the year.
If you have difficulties with written assessments please use the University study skills department: https://www.exeter.ac.uk/departments/tqae/asset/
You will have three written examinations (up to 90 mins) throughout the programme, held under examination conditions. One of these examinations will be formative (for module 1), and the following two will be summative (for modules 1 and 3).
The exam will involve answering multiple choice questions and short answer questions.
Supervisor Practice Outcomes Assessment
A fundamental aspect of the course assessment is the successful completion of competence based practice outcomes supported by your supervisor in practice. To enable you to gain competence in these outcomes, those assigned for each module will all be assessed together at the end of the programme using the Practice Outcomes Assessment document.
Your work-based clinical supervisor will have undertaken a training course detailing the requirements of this aspect of the assessment. In addition they will have gained an understanding of the content and structure of the programme. This will enable them to provide supervision that provides a bridge between your training and your clinical practice.
Role of the Clinical Supervisor
As well as providing general support, the role of the Clinical Supervisor involves monitoring and assessing the developing clinical skills of the student through a variety of methods. These could include direct observation, the use of audio tapes of clinical interviews undertaken by the student and reflections by the student on their developing practice. The taught practice time and Clinical Supervision are essential to the achievement of the clinical practice outcomes in the programme. These are assessed by the supervisor and recorded in the clinical practice outcomes assessment document. The Clinical Supervisor will therefore act to guide and assess the student’s developing knowledge and skills, and the achievement of the clinical practice outcomes in relation to clinical, patient based aspects of the student’s role.
Completion of Practice Outcomes
Whilst your work-based clinical supervisor will support you during the programme and has responsibility for assessing your practice based outcomes it is your responsibility to ensure that you successfully complete the Practice Outcomes Assessment document by the completion date. Failure to do this by the completion date will result in a fail.
Clinical Portfolio
At the end of the programme each student is required to submit a clinical portfolio. This clinical portfolio forms one of the required assessments for all three modules. It also meets the CYP IAPT curriculum requirements. We encourage you to complete the paperwork on an ongoing basis in your portfolio.
Mitigation Requests
Application for mitigation of assessment should be made prior to the assessment deadline in question. Students are responsible for making applications for mitigation to the Programme Administrator for the affected module/element of assessment.
Students may apply for mitigation for more than one module where the same circumstances have affected more than one assessment. However, students must use the correct mitigation form and be explicit in detailing: the circumstances that have affected them, how these circumstances have affected their performance and evidence to support their application (doctor's note etc.)
Students wishing to apply for mitigation for the EEBP course should complete the and return it to the administrator via email. All fields of the form must be completed and a specific, weekday date by which the work is expected to be completed (which doesn't fall on a University of Exeter closure day e.g. - bank holidays) should be provided.
We require both the completed form and evidence to process your request and forward to the mitigation committee who consider mitigation requests.
Please complete the mitigation form fully and ensure that you provide accompanying evidence to support your claim.
Submit this to: CEDAR-mitigations@exeter.ac.uk
You will be required to submit four reflective summaries of 1000 words (N.B. marking will stop at 1000 words):
- Engagement and Assessment Module – with your formative and summative tapes
- Intervention module – with your formative and summative tapes
We would expect you to identify the area that you are going to reflect on and then provide a reflective analysis of this area followed by a plan. Your analysis should demonstrate your ability to reflect on your practice in relation to the CYP IAPT Principle(s) and CBT or other appropriate psychological theory. The analysis should provide a critical evaluation of the therapy skills that you demonstrate within the applying these principles, drawing on relevant theory, research and literature and identify areas for improvement. The following model may be help with this. You should make reference to your self-rating forms within the summary.
The four stage experiential learning model (Kolb 1984 and Lewin 1946) in Bennett-Levy et al (2004 p. 19) is the most widely used model in adult education (see fig. 1).
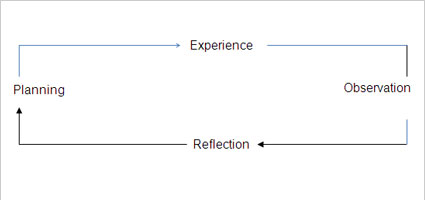
Figure 1.Experiential learning cycle (Bennett-Levy et al. 2004
Different terms have been used by different authors to reflect the same four stages. Plan, Experience, Observe, and Reflect. Effective learning is said to proceed through a series of these cycles:
Experience: The experience
Observe: What happened
Reflect: Making sense of what happened by:
- Relating it to previous experience and knowledge
- Searching for understanding
- Generalising abstracting principles
- Fit with the formulation
Plan: With the new understanding, how can I take this forward?
The purpose of the Reflective Commentary is to demonstrate your ability to:
- Reflect on your experience of EEBP practice
- Critically analyse and make sense of that experience (informed by CBT or psychological theory and literature where appropriate)
- Extract useful learning and plan for change
| Introduction of topic of reflection |
|
|
Experience and observation |
|
|
Critical analysis |
|
|
Understanding and use of theory |
|
| Summary and implications for future practice |
|
| Structure & style |
|
| Spelling / Grammar / Typos |
|
Useful Forms:
Key texts
- Addis, M.E & Martell, C.R. (2004) Overcoming Depression One Step at a Time. (Self-help workbook) Canada. New Harbinger.
- Bennett-Levy, J., Richards, D., Farrand, P. And Christensen, H., Griffiths, K., Kavanagh, D., Klein, B., Lau, M.A., Proudfoot, J., Ritterband, L., White, J. And Williams, C. (2010). Oxford Guide to Low Intensity CBT Interventions. Oxford: Oxford University Press.
- Bennett-Levy, J., Butler, G., Fennell, M., Hackmann, A., Mueller, M., & Westbrook, D. (2004).Oxford guide to behavioural experiments in cognitive therapy. Oxford: Oxford University Press.
- Brent, D, A., Poling, K. L.S.W (1997) Cognitive Therapy Treatment Manual for Depressed and Suicidal Youth. Star Center Publications (for clients aged 13-18years).
- Burton, M. Pavard, E. & Williams B (2014) An Introduction to Child and Adolescent Mental Health. London. Sage.
- Carr, A. (2000). What works with children and adolescents? A critical review of psychological interventions with children, adolescents and their families. London: Routledge.
- Cartwright-Hatton,S., Laskey, B., Rust,S. & McNally, D. (2010) From Timid to Tiger. A Treatment Manual for Parenting the Anxious Child. Chichester. Wiley
- Cooper,M., Hooper,C. & Thompson M. (2005) Child and Adolescent Mental Health. Theory and Practice. London. Hodder Arnold.
- Dogra, N., Parkin. A., Gale, F. and Frake, C. (2002) Child and Adolescent Mental Health for Front-line Professionals. Jessica Kingsley Publishing.
- Friedberg, R.D. & McClure, J.M. (2002). Clinical practice of cognitive therapy with children and adolescents: The nuts and bolts. New York: Guilford Press.
- Fuggle,P., Dunsmuir,S. & Curry,V. (2013) CBT with Children, Young People and Families. London. Sage.
- Gellety, J. et al., (2007). What makes self –helpinterventions effective in the managemtn of depressive symptoms? Mate-analysis and meta-regression. Psychological Mediceine, 37, p. 1217-1228
- Graham,P. (2005) Cognitive Behaviour Therapy for Children and Families. (2nd edition). Cambridge University press.
- Grant, A., Mills,J., Mulhern, R., & Short, N. (2004) Cognitive Behavioural Therapy in Mental Health Care London. Sage Publications.
- Greenberger, D., & Padesky, C.A. (1995). Mind over mood: A cognitive therapy treatment manual for clients. New York: Guildford Press.
- Greenberger, D., & Padesky, C.A. (1995). Mind over mood: A cognitive therapy treatment manual for clients. New York: Guildford Press.
- IMPACT Trial (2010) A manual for the delivery of CBT in the treatment of young people with depression (unpublished draft).
- Kedar, N.D. and Harper, P.B. (2004) Promoting the Emotional Well-being of Children and Adolescents and Preventing Their Mental Ill Health. Jessica Kingsley Publishing
- Kendall, P.C. (2006). Child and adolescent therapy: Cognitive-behavioural procedures. New York: Guilford Press.
- Kendall, P.C. & Hedtke, K.A. (2006) The Coping Cat Workbook (2nd Edition). Workbook Publishing.
- Kendall, P.C. & Hedtke, K.A. (2006) Cognitive Behavioural Therapy for Anxious Children: Therapist manual. Workbook Publishing.
- Kinsella, P. & Garland, A. (2008). Cognitive Behavioural Therapy for Mental Health Workers – a beginner’s guide. Routledge. London.
- Lejuez, C.W., Hopko, D.R., Hopko, S.D. (2001). A brief behavioral activation treatment for depression: Treatment manual. Behavior Modification 25: 255-286. Richards, D. (unpublished) Case management for Depression
- Lovell, K., Richards, D. and members of the MRC Guided Self Help team (unpublished) MRC Self help coach (facilitators manual)
Training and service manuals developed by Professor David Richards
Training protocols developed by Dr Judy Lebiowitz for Camden and Islington NHS guided self help programme - March, J.S., & Mulle, K. (1998). OCD in children and adolescents: A cognitive-behavioural treatment manual. New York: Guilford Press.
- Martel, C.R., Addis, M.E., and Jacobson N.S. (2001) Depression in Context; Strategies for Guided Action New York: W WNorton adapted for adolescents Ritschel and Ramirez (2011). Behavioral Activation for Depressed Teens: A Pilot Study. Cognitive and Behavioral Practice 18, 281–299
- Martell, C. R., Addis, M. E., & Jacobson, N. S. (2001).Depression in context: Strategies for guided action. London: Norton.
- Martell, C.R., Dimidjian, S., & Herman-Dunn, R. (2010). Behavioral Activation for depression: A clinician’s guide. Guilford: New York.
- Milne, D. (2008). Discovering CBT supervision.Wiley, Blackwell.
- Myles, P. and Rushforth, D., 2007. A complete guide to primary care mental health. London: Robinson
- Richards, D. and Wyhte (2008) Stepped care for common mental health probems: a handbook for low intensity workers. Oxford: Wiley (in Press)
- Roth, A. & Fonagy, P. (2006). What Works for Whom? (2nd edition). Guildford Press. New York
- Stallard, P. (2002). Think good, feel good: A cognitive behaviour therapy workbook for children and young people. Chichester: John Wiley & Sons.
- Stallard, P. (2002). A clinicians guide to think good, feel good: Using CBT with children and young people. Chichester: John Wiley & Sons.
- Stallard, Paul. (2009) Anxiety – Cognitive Behaviour Therapy with Children and Young People. Routledge. New York.
- Verduyn, C. Rogers, J. & Wood, A. (2009). Depression – Cognitive Behaviour Therapy with Children and Young People. Routledge. New York
- Westbrook, D. et al. (2007). An Introduction to Cognitive Behaviour Therapy. London. Sage.
- Webster-Stratton, C. (2004). How to Promote Children’s Social and Emotional Competence (Seventh Edition). London: Sage Publications.
- Webster-Stratton, C. & Herbert, M. (2000). Troubled Families – Problem Children: Working with Parents: A Collaborative Process (Sixth Edition). Chichester: Wiley.
- Williams, C. 2003. Overcoming anxiety: a five areas approach. London: Arnold.
- MindEd sessions (see Curriculum)
NICE Guidelines
CG22
National Institute for Health and Clinical Excellence. (2004). Anxiety: management of anxiety (panic disorder, with or without agoraphobia, and eneralized anxiety disorder) in adults in primary, secondary and community care. London: NICE.
CG113
National Institute for Health and Clinical Excellence. (2011). Generalised anxiety disorder and panic disorder (with or without agoraphobia) in adults: management in primary, secondary and community care (partial update). London: NICE.
CG28
National Institute for Health and Clinical Excellence. (2005). Depression in children and young people: identification and management in primary, community and secondary care. London: National Institute for Health and Clinical Excellence.
CG31
National Institute for Health and Clinical Excellence. (2005). Obsessive Compulsive Disorder: core interventions in the treatment of obsessive compulsive disorder and body dysmorphic disorder. London: NICE.
CG 026
National Institute for Health and Clinical Excellence. (2005). Post-traumatic Stress Disorder: the management of PTSD in adults and children in primary and secondary care. London: Royal College of Psychiatrists and British Psychological Society.
TA102
National Institute for Health and Clinical Excellence. (2006). Parent-training/education programmes in the management of children with conduct disorders. London: National Institute for Health and Clinical Excellence.
Key Websites
- http://www.camhsnetwork.co.uk
- http://www.cypiapt.org/children-and-young-peoples-project.php?accesscheck=%2Findex.php
- http://www.iapt.nhs.uk/workforce/supervisors
- https://www.minded.org.uk
- http://www.ucl.ac.uk/CORE
- NHS Health and social care bill 2011: http://www.dh.gov.uk/en/Publicationsandstatistics/Legislation/Actsandbills/HealthandSocialCareBill2011/index.htm
- No Health without Mental Health: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_123766
- Roth & Pilling (2007) & Roth, Calder & Pilling (NHS Education for Scotland Competence Framework for Workers in CAMHS Settings, 2011): http://www.ucl.ac.uk/clinical-psychology/CORE/competence_frameworks.htm
- Turpin & Wheeler (2011): http://www.iapt.nhs.uk/silo/files/iapt-supervision-guidance-revised-march-2011.pdf
- Referencing: http://owl.english.purdue.edu/owl/resource/560/08/
Throughout the course trainees will receive supervision from workplace based supervisors. Should there be any difficulties that arise within your supervisory relationship, in the first instance please try to work with your supervisor to address these. If difficulties continue, please discuss this with your manager, 1:1 tutor or the Programme Lead.
1. Supervision and cases:
As part of the programme you will receive weekly group supervision with your service supervisor (the equivalent of 30 mins per trainee). You need to receive a minimum of 15 hours of supervision over the course.
You need to complete 40 hours of clinical practice over the course of the year. You will need to see at least three completed cases (seen for 5 sessions or more from start to completion/termination). Two of these cases will need to be anxiety presentations, and one case a depression presentation. With one of the cases, you will also need to evidence working with parents as part of your intervention.
We have provided a supervision contract for you and your supervisor to work through during your initial meetings to help you discuss and agree the nature and content of your supervision. This will form the Supervision Contract between yourself and your Workplace Supervisor. Please do adapt this to your individual needs if helpful, it is only meant to be a suggested format.
2. Supervision Feedback
We have provided the BABCP’s supervisee feedback form on supervision which can be a useful tool to help you review supervision with your supervisor at the end of each term. At the end of each supervision session we will ask you to provide feedback to your supervisor by using the Helpful Aspects of Supervision Questionnaire (HASQ). This should be reviewed on an ongoing basis with your supervisor and we would encourage you to give accurate and constructive feedback using this tool so that you can gain the most from your supervision sessions over the course of the year.
3. Your Supervisors
Your supervisor will provide you with intensive skills-based supervision, helping to develop your CBT competencies and theory practice links. They will supervise a minimum of 3 cases over the course. Your Workplace based supervision will also involve caseload supervision. They will hold an overview of all your clinical cases for the course.
Your supervisor will have expertise in CBT and will have undertaken the CYP IAPT supervision training (either the Generic Outreach Supervisor Training or PG Cert in Supervising Evidence Based Psychological Therapies). They will be offered training in the requirements of supervision and the clinical assessment associated with the programme. They will also be offered ongoing continued professional development (CPD) and supervision of supervision.
4. Your Role as Supervisee
In addition to filling in the clinical and supervision logs and reports (see below) you will also need to think about your role as a supervisee. This will include coming prepared for your supervision (see supervision preparation form), keeping notes on discussions in supervision and carrying through jointly agreed action points (see record of supervision) and bringing a summary of your supervision to your 1:1 tutorials (see ongoing summary of supervision hours).You will also be expected to bring weekly video clips of your session with your clients. If you have any concerns about your cases or supervision please do raise these with your supervisors in the first instance.
5.Guidance on the use of Supervision
In order to ensure that you make the most effective use of supervision we suggest you read the guidance included in this handbook. In addition we have included below some suggested content of supervision and supervision methods and topics.
Content of supervision
- Content of supervision will focus on the acquisition of knowledge, conceptualisation and clinical skills within a cognitive behavioural model(s).
- Associated issues will also be discussed when it is relevant to do so e.g. medication, hospitalisation, case management.
- Identification (and collaborative change of these if appropriate) of supervisee thoughts, attitudes, beliefs and values and the impact of these on therapeutic and professional behaviour.
- Discussion and working through relationship and process aspects of supervision.
Supervision methods and topics
- Discussion of therapeutic relationship and engagement issues.
- Case conceptualisation/formulation.
- Rehearsal of therapeutic techniques e.g. simulation, role-play.
- Discussion about therapeutic strategies.
- Case Presentations.
- Homework.
- Review of audio and videotapes*
- Direct observation of practice
- Identification of supervisee thoughts, attitudes, beliefs with exploration of the impact of these on therapeutic and professional behaviour.
- Review of risk and therapist/service user safety.
- Review of clinical guidelines/manuals.
- Review of psychoeducational material.
- Experiential exercises.
- Other strategies as agreed.
6. Liaison between Supervisor and University – Progress Reviews
There will be regular liaison between the work-based supervisor and the University to ensure the trainee is on track. Should there be concerns, the work-based supervisor is encouraged to contact the University so that a plan can be put in place, if necessary. A mid-programme Review Meeting will also take place to discuss how the trainee is progressing and to review the Practice Outcomes document. The structure for the Review meetings (progress review form) is set out below.
Template Forms
Files to download:
- Cover Sheet for Formative/Summative EEBP Competency Assessment Recording
- Consent to Record Form for Parents and Young People (EEBP)
- Criteria for EEBP Competency Assessment Session (Marksheet)
- Criteria for EEBP Competency Intervention Session (Marksheet)
- Criteria for EEBP Reflective Summary (Marksheet)
- 1:1 Tutorial Termly Review (.pdf)
- EEBP Clinical Practice Outcomes Assessment
EEBP Supervision Forms
Files to download:
- EEBP Supervision Contract
- Supervision Preparation Form
- Progress Review Form
- Record of Supervision Form
- Supervisee Feedback Form
- Summary of Supervision, Supervised Practice and Cases Form
- HASQ Form
EEBP Clinical Portfolio Forms
Files to download:
- Clinical Portfolio Front Sheet
- Summary of Supervision, Supervised Practice and Cases Form
- Clinical Log of Cases
- Client Summary Sheet
- Supervision Log
- Teaching Log
- Self-reflection Hand-out
Other Useful Resources: