Assessment Overview - Cohort 14
Academic Honesty: Please read this document about academic honesty before submitting any assignments. The mandatory academic honesty and plagiarism module and quiz can be found on ELE.
Please note for submissions that require a consent form, the consent form must also be submitted by the submission deadline. If you believe you have grounds for an extension, please see the Mitigations drop-down section below.
C14 Course assessment flowchart
Assessment Overview by Module
| Module Code | Module Name | Assessment | % Marks | Deadline Dates |
| PYCM040 | CBT Clinical Practice | Assessment & Formulation Case Presentation | 50% | 20th September 2021 |
| PYCM039 | CBT for Anxiety Disorder | Essay | 33% | 18th October 2021 |
| PYCM039 | CBT for Anxiety Disorder | Case Report | 33% | 22nd November 2021 |
| PYCM039 | CBT for Anxiety Disorder | Competency Tape and Reflective Summary | 34% | 3rd December 2021 |
| PYCM038 | CBT Depression | Depression Essay | 33% | 7th March 2022 |
| PYCM038 | CBT Depression | Depression Case Report | 33% | 28th March 2022 |
| PYCM038 | CBT Depression | Competency Tape and Reflective Summary | 34% | 1st April 2022 |
| PYCM037 | Fundamentals of CBT | Self Practice/Self Reflection Summary | 10% | 9th May 2022 |
| PYCM037 | Fundamentals of CBT | Extended Case Report | 90% | 23rd May 2022 |
| PYCM040 | CBT Clinical Practice | Anxiety Disorder 2 Competency Tape & Reflective Summary | 50% | 27th May 2022 |
| PYCM040 | CBT Clinical Practice | Clinical Portfolio including Supervisors Reports | Pass/Fail | 8th July 2022 |
More information
Summative assessments contribute to your final mark for a module. They are marked according to the assessment criteria and intended learning outcomes of a module.
Formative assessments do not contribute to your final mark given for a module, but provide feedback that is an integral part of your learning.
| Term | Assessment | Formative or Summative |
Submission Date |
How to submit/hand in |
|---|---|---|---|---|
| 1 | Self-Rated CBT Competency (CTS-R & Reflection) | Formative | Tuesday 24th August 2021 |
You should submit the formative competency tape in the way that you would submit the summative tapes:
Competency tape via secure University sharepoint. Consent to Recording form needs to be sent separately to the programme administrator. Cover sheet with student signature, Formulation, CTSR Scale and Reflective Summary all to upload to secure University sharepoint.
|
| Formative group case presentation | Formative | Tuesday 31st August | Group presentation pre-recorded video submitted to secure University sharepoint. Client consent form to be emailed separately to programme adminstrator. | |
| 2 | PYCM040 Assessment & Formulation Case Presentation | Summative | Monday 20th September 2021 | Pre-recorded video of presentation submitted to secure University sharepoint. PDF version of presentation slides via eBART. Case presentation cover sheet required with student and workplace supervisor signature via eBART. Client consent form to be emailed separately to programme adminstrator. |
| CTS-R, self-rating and reflective summary within supervision | Formative | To be agreed with supervisor | Competency tape via secure sharing method within supervision or approved service portal. Reflection emailed to supervisor. | |
| PYCM039 Anxiety Essay | Summative | Monday 18th October 2021 | eBART (pdf). Essay cover sheet required with student signature via eBART (pdf) | |
| PYCM039 Anxiety Case Report | Summative | Monday 22nd November 2021 | Cover sheet required with student and workplace supervisor's signatures & Case Report via eBART (pdf). Client consent form to be emailed separately to programme adminstrator. | |
| PYCM039 Competency Tape and Reflective Summary | Summative | Friday 3rd December 2021 | Competency tape via secure University sharepoint. Consent to Recording form needs to be sent separately to the programme administrator. Cover sheet with student signature, Formulation, CTSR Scale and Reflective Summary all to upload to secure University sharepoint. | |
| Supervisors reports | Formative | Monday 6th December 2021 by 11am | Via eBART (pdf). | |
| 3 | CTS-R, self-rating and reflective summary within supervision | Formative | To be agreed with supervisor | Competency tape via secure sharing method within supervision or approved service portal. Reflection emailed to supervisor. |
| PYCM038 Depression Essay | Summative | Monday 7th March 2022 | eBART (pdf). Essay cover sheet required with student signature via eBART (pdf) | |
| PYCM038 Depression Case Report | Summative | Monday 28th March 2022 | Cover sheet required with student and workplace supervisor's signatures & Case Report via eBART (pdf). Client consent form to be emailed separately to programme adminstrator. | |
| PYCM038 Depression Competency Tape and Reflective Summary | Summative | Friday 1st April 2022 | Competency tape via secure University sharepoint. Consent to Recording form needs to be sent separately to the programme administrator. Cover sheet with student signature, Formulation, CTSR Scale and Reflective Summary all to upload to secure University sharepoint. | |
| Supervisors reports | Formative | Monday 4th April 2022, by 11am | Via eBART (pdf) | |
| 4 | PYCM037 Self Practice/Self Reflection Summary | Summative | Monday, 9th May |
Via eBART (pdf) with cover sheet with student's signature. |
| PYCM037 Extended Case Report | Summative | Monday 23rd May |
Cover sheet required with student and supervisor's signatures & Case Report via eBART (pdf). Client consent form to be emailed separately to programme adminstrator. |
|
| PYCM040 Competency Tape and Reflective Summary | Summative | Friday 27th May |
Competency tape via secure University SharePoint. Consent to Recording form needs to be sent separately to the programme administrator. Cover sheet with student signature, Formulation, CTSR Scale and Reflective Summary all to upload to secure University SharePoint. |
|
| Supervisors' Reports | Summative | Monday 30th May 2022, by 11am |
Via eBART (pdf). Copy to be included in Clinical Portfolio. |
|
| PYCM040 Clinical Portfolio | Summative | Friday 8th July |
TBA |
1:1 Tutorial Dates
- Term 2 - 17th September
- Term 3 - 11th February
- Term 4 - 20th May or 23rd May
Supervisors Reports
Over the course of the year, you will be required to hand in three supervisors reports by both your University and Workplace Supervisors, one in term 2, one in term 3 and one in term 4. The reports handed in in terms 2 and 3 are formative reports. The University and Workplace supervisors reports handed in in term 4 are summative and a copy must also be included in your PYCM040 Clinical Portfolio.
| Name of Assessment |
Deadline Dates |
| Formative University & Workplace Supervisors Report - term 2 |
Monday 6th December 2021 by 11am |
| Formative University & Workplace Supervisors Report - term 3 |
Monday 4th April 2022 by 11am |
| Summative University & Workplace Supervisors Report - term 4 |
Monday 30th May 2022 by 11am |
You must submit all of your supervisors reports (six in total) via eBART. We do not need hard copies of these reports. You should keep the original copies.
Resubmissions
If you receive a mark below 50%, this is classed as a fail and you will need to resubmit your assignment. You will have four weeks to resubmit your assignment (up to 12 weeks for CTSR resubmissions).
Please note that where assessments for part or all of a module are referred the whole module must be capped at 50% for postgraduate modules.
Resubmitted work should be submitted alongside:
1. A copy of the previous marking feedback
2. A resubmission cover sheet that shows how you have addressed the issues identified. Please see the Forms section below.
Assessment Information
For details on late submission policies please see the CEDAR PGT generic handbook.
Please refer to your ELE page for further information.
You will need to submit two essays during the course.
CBT for Anxiety Disorders PYCM039
Submission date: Monday 18th October 2021 at 1pm
Word limit: 3,750
NB marking will stop at this word limit and work exceeding this limit will therefore not receive credit
Essay Title:
'Remote delivery of CBT for anxiety disorders should be the treatment method of choice'.
Critically evaluate this statement with reference to theory, empirical literature, and any implications for both Cognitive Behavioural Therapy and clinical practice in IAPT services. Please illustrate your argument with reference to one or two specific anxiety disorders, including a model and interventions for the disorder/s.
Having read the literature you may decide that you agree with this statement, disagree with the statement or remain in two minds - whatever your conclusion, we expect you to support your argument with evidence from empirical studies. You may also wish to draw on clinical examples.
CBT for Depression PYCM038
Submission date: Monday 7th March 2022 at 1pm
Word limit: 3,750
NB marking will stop at this word limit and work exceeding this limit will therefore not receive credit
Essay title:
To what extent does the efficacy of CBT for depression depend upon individual patient characteristics? Your answer should demonstrate an understanding of cognitive behavioural theory of depression, include reference to empirical studies and comment upon the implications for clinical practice and IAPT services.
For guidance on submitting written work please refer to the University Guidance on written work in the IAPT Programmes Handbook. If you have difficulties with written assessments please use the University study skills department.
Essay Guidelines
You will be assessed on the following dimensions:
| *Interpretation of title |
|---|
| Marks will be awarded for your ability to answer the essay question posed. Therefore ensure you read the essay question clearly and that you understand it; if not ask. In order to pass this section you will need to clearly address all elements of the essay question. |
| *Understanding of theory |
| Marks will be awarded where you demonstrate a clear understanding of relevant theory and the ability to apply this understanding to answer the essay question. |
| *Critical analysis |
| Marks will be awarded where you demonstrate an ability to not only pull together relevant information but also to analyse this critically, for example weighing it against evidence that does not fit with the point you are making and demonstrating a thoughtful reflective approach or commenting on the rigor of the evidence cited. You should clearly differentiate your own opinions from those critiques reported from the work of other authors. |
| *Summary of arguments & implications |
| Marks will be awarded where you demonstrate an ability to summarise your arguments and comment on the implications they may have for clinical practice and or future research. The essay should not be a purely theoretical exercise and it is important that you demonstrate your ability to apply your conclusions to the broader context within which you are working. |
| Use of sources |
| You need to ensure that the points you make are backed up by relevant literature. We would expect you to use a wide source of references e.g. journals, books and websites. An absolute minimum of 10 references would be the norm. |
| Structure & style |
| Marks will be awarded for a well-structured essay. The essay should flow well with a clear introduction (including essay plan), middle and end. Make use of summaries to help the reader through your arguments. Think about what point you are making and why, make your point and where available support it with evidence, and then reflect and summarise the point. Be mindful of your use of language both the use of colloquialisms and jargon. Where appropriate you may use diagrams, tables and bullet points. These should be used to aid clarity. If used, subheadings should relate to subsequent material presented and help to structure your essay. If used, appendices and footnotes should be used appropriately and not to help with word count. Key information needs to be in the main body of the text. Appendices should be clearly referred to and labelled and come after the reference section. |
| References |
| References should conform to APA (7th Edition) both in text and at the end of your essay (see University guidance). Please check references in terms of accuracy and consistency and ensure that all citations in the text are referred to in the reference section. Minor errors with referencing will not impact on the overall mark, however disregard for APA referencing, or severe departures from APA, may impact the overall mark. |
| Spelling, grammar, typographical errors and presentation |
| Work should be double spaced and page-numbered. Work should be comprehensible and so please check for typographical, grammatical and spelling errors. Where possible ask someone else to proof read your essay before submitting. If you need support in this area please use the study skills department. |
| Word count |
|
Word count excludes: essay title, tables, figures, headings for tables/figures, the reference list, and appendices. All other words are counted. Work exceeding this limit will not be marked and will not receive credit. |
* Indicates a key area; failure on more than one of these areas is likely to result in an overall fail.
Case Presentation and Case Report Marking Criteria
Please also refer to University guidelines on written material.
| Range | Assessment and Formulation Case Presentation | Anxiety and Depression Case Reports | Extended Case Report |
|---|---|---|---|
| Distinction 70-100% |
Work of exceptional standard reflecting outstanding competence/knowledge of material and critical ability above and beyond those required for a pass mark. | As in Assessment and Formulation Case Presentation | As in previous Case Reports |
| Merit 60-69% |
Work with a well-defined focus, reflecting a good working competence/knowledge of material and a good level of competence in its critical assessments and beyond those required for a pass mark. | As in Assessment and Formulation Case Presentation | As in previous Case Reports |
| Pass 50-59% |
Work demonstrating adequate competence/working knowledge of material and evidence of some analysis. Work adheres to the relevant NICE guideline. A piece of work in this category should include the following (unless a clear rationale for exceptions is given): Reason for selecting this case, the presenting problems should be clearly identified and described with goals for therapy included. Where available an appropriate model should be used. The assessment should include factors relevant to the development and maintenance of the difficulties. Where appropriate the relevant disorder specific assessment and outcome tools should be used as well as IAPT required measures. A formulation should be present in written narrative form as well as a diagram (if possible). This formulation should flow logically from assessment and include precipitating and maintaining factors and where appropriate predisposing/developmental factors. The intervention plan should be clearly described and flow logically from formulation. There should be some critical analysis and reflection on the work and the therapeutic alliance. Throughout the presentation, a professional and ethical stance should be demonstrated. References and awareness of relevant literature generally accurate but limited. Adheres to time limit. |
As in Assessment and Formulation Case Presentation and additionally:
Adheres to word count. |
As in previous Case Reports and additionally:
The intervention work must be completed. |
| Condonable Fail 40-49% |
Limited competence/knowledge of core material and limited critical ability. Poorly written and presented/structured piece of work. Rationale and arguments are absent or problematic. Inappropriate application of theory to practice. Severe departures from APA referencing. | As in Assessment and Formulation Case Presentation | As in previous Case Reports |
| Fail 0-39 |
Lacking in basic competence/knowledge of core material and absence or major flaws in critical analysis. Unethical practice, breaches in confidentiality** |
As in Assessment and Formulation Case Presentation | As in previous Case Reports |
Assessment and Formulation Case Presentation
Trainees give one summative case presentation. This should be pre-recorded and submitted, along with the slides/resources. The case presentation can be of a client with either anxiety or depression and should be a non-closely supervised client. The presentation needs to be of the same client being used for the formative competencies assessment (CTS-R) submission at the end of term 1. Please note trainees should not use this case presentation client for any other formative or summative assignment. This means that this client cannot be used for any of the summative case reports.
Trainees also have the opportunity to practise giving a case presentation prior to this, by giving a formative group presentation on the assessment, formulation and intervention plan of a specific client one of the group members is working with. The cases used for the formative and summative case presentations need to be different. Markers will give formative feedback on these presentations to the wider group, to help trainees prepare for the summative case presentations in term 2. It is recommended that trainees familiarise themselves with the case presentation guidance in the handbook and follow a similar structure to that which will be used for the summative case presentations.
The purpose of the case presentation is to demonstrate trainees’ grasp of the application of cognitive theory to clinical practice and to demonstrate their skills in assessment and formulation.
Trainees need to use anonymised biographical data throughout the presentation - no identifiable information should be presented on the client or the service. i.e. change any names and identifying information**
Trainees are marked on the content of their case presentation rather than on their presentation skills.
Guidelines
Trainees will be assessed on the following dimensions:
| *Assessment |
|---|
|
Should include:
|
| *Conceptualisation / Formulation |
|
| *Intervention Plan |
The intervention plan should:
|
| *Link of theory to practice |
|
This is covered to some extent in previous areas. Within the presentation you will need to evidence a satisfactory understanding of the relevant cognitive-behavioural theory and disorder specific model. This should be described in sufficient detail prior to presenting the idiosyncratic formulation and planned intervention.
|
| Self reflectivity |
| Throughout the presentation you should demonstrate a reflective approach to the work you carried out and the use of methods/tools to aid this process. For example we would expect you to provide a rationale for the work carried out that draws on your ability to reflect on theory/therapeutic alliance/socio/political/organisational/professional and ethical factors. Reflection may involve demonstrating an awareness of the way that your own assumptions/beliefs might impact on the process and outcome of therapy with due consideration of how this may shape and develop your practice in the future. You may find it helpful to provide an outline of any tools or mechanisms that you used in order to aid this process (e.g. supervision discussion, protected preparation time for therapy & supervision sessions, a reflective model, thought records, listening to session recordings etc.). |
| Awareness of professional issues (including confidentiality) |
Your work should demonstrate good professional awareness, e.g. awareness of:
|
| Structure and style of presentation |
| Marks will be awarded for a well-structured and well-presented case presentation. Use of PowerPoint is encouraged. The case presentation should flow in a logical manner and any slides/hand-outs provided should be relevant and aid the marker. Be mindful of your use of language, both regarding the use of colloquialisms and jargon. Where appropriate you may make use of diagrams, tables and bullet points in the presentation to clarify information. Diagrams of the case conceptualisation can be provided on a separate handout or included in the slides. A possible structure could be based on the marking criteria e.g.: Introduction to the presentation, reason for referral, presenting problem(s), assessment, formulation, intervention plan and critical evaluation/discussion. Theory to practice links, self-reflectivity and professional issues could be covered throughout the presentation. An introduction should be included, clearly outlining the structure of the case presentation and material to be covered. Your case presentation should be clearly presented and you may wish to consider practising your presentation before you record it where possible. |
| References |
| References should be given throughout the presentation slides and provided in a reference section at the end. References should conform to APA (7th Edition) - see University guidance. Please check references in terms of accuracy and consistency and ensure that all citations in the slides are referred to in the reference section. Minor errors with referencing will not impact on the overall mark, however disregard for APA referencing, or severe departures from APA, may impact the overall mark. |
| Spelling, grammar, typographical errors |
| The information in your slides should be comprehensible and so please check for typographical, grammatical and spelling errors. Where possible ask someone else to proof read your slides before submitting. If you need support in this area please use the study skills department. |
| Length of Presentation |
| The case presentation should be a maximum of 20 minutes’ duration. Marking will stop at 20 minutes and information not presented will not receive credit. |
* Indicates a key area; failure on more than one of these areas is likely to result in an overall fail.
** Confidentiality breaches in case presentations:
- With Case Presentations, no identifiable information shuold be presented on the Client or the Service.
- A minor breach in Case Presentations, where confidentiality/anonymisation has occurred and been acknowledged by the author, but then a minor mistake(s) gets picked up will be returned to the author for correction. The Trainee will have 48 hours (excluding weekends) to reply and correct the errors in the presentation handouts, otherwise it will be marked as a fail. The Trainee will be notified via their University email account by the Programme Administrator. If the breach occurs during a vacation period, then they will also receive an alert to their work and personal email addresses (where these have been provided) asking them to urgently check their University accounts.
- When major breaches are present or anonymisation has not occurred and/or been made explicit, this will be an automatic fail and the Trainee would need to resubmit a second submission correcting the error (and making any other changes if there are any other resubmission criteria).
Case Presentation and Case Report Marking Criteria
Please also refer to University guidelines on written material.
| Range | Assessment and Formulation Case Presentation | Anxiety and Depression Case Reports | Extended Case Report |
|---|---|---|---|
| Distinction 70-100% |
Work of exceptional standard reflecting outstanding competence/knowledge of material and critical ability above and beyond those required for a pass mark. | As in Assessment and Formulation Case Presentation | As in previous Case Reports |
| Merit 60-69% |
Work with a well-defined focus, reflecting a good working competence/knowledge of material and a good level of competence in its critical assessments and beyond those required for a pass mark. | As in Assessment and Formulation Case Presentation | As in previous Case Reports |
| Pass 50-59% |
Work demonstrating adequate competence/working knowledge of material and evidence of some analysis. Work adheres to the relevant NICE guideline. A piece of work in this category should include the following (unless a clear rationale for exceptions is given): Reason for selecting this case, the presenting problems should be clearly identified and described with goals for therapy included. Where available an appropriate model should be used. The assessment should include factors relevant to the development and maintenance of the difficulties. Where appropriate the relevant disorder specific assessment and outcome tools should be used as well as IAPT required measures. A formulation should be present in written narrative from and also a diagram if possible. This formulation should flow logically from assessment and include precipitating and maintaining factors and where appropriate predisposing/developmental factors. The intervention plan should be clearly described and flow logically from formulation. There should be some critical analysis and reflection on the work and the therapeutic alliance. Throughout the report, a professional and ethical stance should be demonstrated. References and awareness of relevant literature generally accurate but limited. Adheres to time limit. |
As in Assessment and Formulation Case Presentation and additionally:
Adheres to word count. |
As in previous Case Reports and additionally:
The intervention work must be complete. |
| Condonable Fail 40-49% |
Limited competence/knowledge of core material and limited critical ability. Poorly written and presented/structured piece of work. Rationale and arguments are absent or problematic. Inappropriate application of theory to practice. Severe departures from APA referencing. | As in Assessment and Formulation Case Presentation | As in previous Case Reports |
| Fail 0-39 |
Lacking in basic competence/knowledge of core material and absence or major flaws in critical analysis. |
As in Assessment and Formulation Case Presentation | As in previous Case Reports |
Case Reports
Trainees submit three case reports over the year on three different clinical cases. Trainees also present one case as a case presentation during the year which must also be on a different case.
One Anxiety and One Depression Case Report (4,000 words each)
Aims
The purpose of these case reports is to demonstrate your grasp of the application of cognitive theory to clinical practice.
Extended Case Report (7,000 words)
This can be of a client with either anxiety or depression. The client used for the extended case report can be any of the 8 closely- or non-closely supervised cases (either depression or anxiety) which have not been used for any other case report or the summative case presentation previously. For the Extended Case Report, the intervention work must be complete.
Aims
The overall aims of the extended case report are for you to demonstrate your grasp of the application of cognitive theory to clinical practice by demonstrating an understanding of evidence-based practice and providing a critical discussion of the relevant research/literature evidence to this case.
You will be required to reflect on one or two key themes or issues that were apparent or relevant to this case and discuss these with reference to relevant research/literature. You may wish to include transcript of sessions with this client to illustrate your points and provide material for reflection. The area chosen may relate to any area of CBT and clinical work. Examples might include cultural or diversity issues, different cognitive-behavioural models, process issues, issues relating to the therapeutic alliance, contextual or systemic factors, co-morbidity.
NB A good case does not necessarily mean one with a good outcome
We require you to demonstrate not just your application of CBT theory to clinical practice but also your reflections and learning related to this piece of clinical work and your understanding of evidence-base practice.
NB In all case reports material presented must reflect accurately the assessment and interventions carried out with the relevant client. If misrepresentations come to light the case report will automatically fail. Case studies submitted should be signed by workplace supervisors to verify that the written piece accurately represents the clinical work carried out.
Anxiety and Depression (4,000 word) Case Report Guidelines
Trainees will be assessed on the following dimensions:
| *Assessment |
|---|
Should include:
|
| *Conceptualisation / Formulation |
|
| *Intervention |
|
| *Critical evaluation/outcome |
|
| *Link of theory to practice |
|
This is covered to some extent in previous areas.
|
| Self reflectivity |
| Throughout the case report you should demonstrate a reflective approach to the work you carried out and the use of methods/tools to aid this process. For example we would expect you to provide a rationale for the work carried out that draws on your ability to reflect on theory/therapeutic alliance/socio/political/organisational/professional and ethical factors. Reflection may involve demonstrating an awareness of the way that your own assumptions/beliefs might impact on the process and outcome of therapy with due consideration of how this may shape and develop your practice in the future. You may find it helpful to provide an outline of any tools or mechanisms that you used in order to aid this process (e.g. supervision discussion, protected preparation time for therapy & supervision sessions, a reflective model, thought records, listening to session recordings, SP/SR etc.). |
| Awareness of professional issues (including confidentiality) |
Your work should demonstrate good professional awareness, e.g. awareness of:
|
| Structure and style |
|
Marks will be awarded for a well-structured case report. The case report should read well and flow in a logical manner. Be mindful of your use of language both the use of colloquialisms and jargon. Trainees should refer to themselves as 'the author' rather than 'I' within academic writing. Where appropriate you may use diagrams, tables and bullet points. These should be used to aid clarity of information in the main text. Key information needs to be in the main body of the text and any information in tables/diagrams needs to be at least summarised within the main text. Key information such as each of the '5 Ps', risk, differential diagnosis, narrative description of the formulation, interventions, critical evaluation, and the theory underpinning the work all needs to be described within the text. If used, subheadings should relate to subsequent material presented and help to structure your case report. If used, appendices and footnotes should be used appropriately and not to help with word count. Appendices should be clearly referred to, labelled and follow the reference section. A possible structure could be based on the marking criteria e.g.: Outline/introduction to the client and the case report, reason for referral, presenting problem(s), assessment, formulation, intervention plan and critical evaluation. Theory to practice links, self reflectivity and professional issues could be covered throughout in the previous sections or as separate sections. |
| References |
| References should conform to APA (7th Edition) both in text and at the end of your case report (see University guidance). Please check references in terms of accuracy and consistency and ensure that all citations in the text are referred to in the reference section. Minor errors with referencing will not impact on the overall mark, however disregard for APA referencing, or severe departures from APA, may impact the overall mark. |
| Spelling, grammar, typographical errors and presentation |
| Work should be double spaced and page-numbered. Work should be comprehensible and so please check for typographical, grammatical and spelling errors. Where possible ask someone else to proof read your case report before submitting. If you need support in this area please use the study skills department. |
| Word count |
| Word count excludes: case report title, tables, figures, headings for tables/figures, the reference list, and appendices. All other words are counted. Work exceeding this limit will not be marked and will not receive credit. |
* Indicates a key area; insufficient information in any of these areas or failure on more than one of these areas is likely to result in an overall fail.
**Confidentiality Breaches in Case Reports:
- In Case Reports there should be no identifiable information in relation to the Client or Service.
- A minor breach in Case Reports, where confidentiality/anonymisation has occurred and been acknowledged by the author, but then a minor mistake(s) gets picked up will be returned to the author for correction. The Trainee will have 48 hours (excluding weekends) to reply and correct the errors, otherwise it will be marked as a fail. The Trainee will be notified via their University email account by the Programme Administrator. If the breach occurs during a vacation period, then they will also receive an alert to their work and personal email addresses (where these have been provided) asking them to urgently check their University accounts.
- When major breaches are present or anonymisation has not occurred and/or been made explicit, this will be an automatic fail and the Trainee would need to resubmit a second submission correcting the error (and making any other changes if there are any other resubmission criteria).
Extended (7,000 word) Case Report Guidelines
Trainees will be assessed on the following dimensions:
| *Assessment | |
|---|---|
Should include:
|
|
| *Conceptualisation / Formulation | |
|
|
| *Intervention | |
|
|
| *Critical evaluation/outcome | |
|
|
| *Link of theory to practice | |
| This is covered to some extent in previous areas. Throughout the report you need to:
|
|
| *Critical appraisal of themes | |
| You need to clearly identify one or two key themes or issues that were relevant to this case (see suggestions above). You should critically appraise:
|
|
| Self reflectivity | |
| Throughout the case report you should demonstrate a reflective approach to the work you carried out and the use of methods/tools to aid this process (e.g. the use of supervision), specifically in relation to your chosen theme(s). For example we would expect you to provide a rationale for the work carried out that draws on your ability to reflect on theory/therapeutic alliance/socio/political/organisational/professional and ethical factors. Reflection may involve demonstrating an awareness of the way that your own assumptions/beliefs might impact on the process and outcome of therapy with due consideration of how this may shape and develop your practice in the future. You may find it helpful to provide an outline of any tools or mechanisms that you used in order to aid this process (e.g. supervision discussion, protected preparation time for therapy & supervision sessions, reflective models, thought records, listening to session recordings, SP/SR etc.). You may wish to include a transcript of sessions with this client to illustrate your points and provide material for reflection. | |
| Awareness of professional issues (including confidentiality) | |
Your work should demonstrate good professional awareness, e.g. awareness of:
|
|
| Structure and style | |
|
Marks will be awarded for a well-structured case report. The case report should read well and flow in a logical manner. Be mindful of your use of language both the use of colloquialisms and jargon. Trainees should refer to themselves as 'the author' rather than 'I' within academic writing. Where appropriate you may use diagrams, tables and bullet points. These should be used to aid clarity of information in the main text. Key information needs to be in the main body of the text and any information in tables/diagrams needs to be at least summarised within the main text. Key information such as each of the '5 Ps', risk, differential diagnosis, narrative description of the formulation, interventions, critical evaluation, the theory underpinning the work and critical appraisal of theme/s all needs to be described within the text. If used, subheadings should relate to subsequent material presented and help to structure your case report. If used, appendices and footnotes should be used appropriately and not to help with word count. Appendices should be clearly referred to and labelled and come after references. A possible structure could be based on the marking criteria e.g.: Outline/introduction to the client, the case report and key themes that will be discussed; reason for referral; presenting problem(s); assessment; formulation; intervention plan; and critical evaluation and reflective analysis. Theory to practice links, critical appraisal of theme/s, self reflectivity and professional issues could be covered throughout in the previous sections or as separate sections. |
|
| References | |
| References should conform to APA (7th Edition) both in text and at the end of your case report (see University guidance). Please check references in terms of accuracy and consistency and ensure that all citations in the text are referred to in the reference section. Minor errors with referencing will not impact on the overall mark, however disregard for APA referencing, or severe departures from APA, may impact the overall mark. | |
| Spelling, grammar, typographical errors and presentation | |
| Work should be double spaced and page-numbered. Work should be comprehensible and so please check for typographical, grammatical and spelling errors. Where possible ask someone else to proof read your case report before submitting. If you need support in this area please use the study skills department. | |
| Word count | |
| Word count excludes: case report title, tables, figures, headings for tables/figures, the reference list, and appendices. All other words are counted. Work exceeding this limit will not be marked and will not receive credit. |
* Indicates a key area; insufficient information in any of these areas or failure on more than one of these areas is likely to result in an overall fail.
**Confidentiality Breaches in Case Reports:
- In Case Reports there should be no identifiable information in relation to the Client or Service.
- A minor breach in Case Reports, where confidentiality/anonymisation has occurred and been acknowledged by the author, but then a minor mistake(s) gets picked up will be returned to the author for correction. The Trainee will have 48 hours (excluding weekends) to reply and correct the errors, otherwise it will be marked as a fail. The Trainee will be notified via their University email account by the Programme Administrator. If the breach occurs during a vacation period, then they will also receive an alert to their work and personal email addresses (where these have been provided) asking them to urgently check their University accounts.
- When major breaches are present or anonymisation has not occurred and/or been made explicit, this will be an automatic fail and the Trainee would need to resubmit a second submission correcting the error (and making any other changes if there are any other resubmission criteria).
Assessment of Clinical Skills / CBT Competencies via Formative and Summative asessments using the CTS-R for recordings of clinical sessions submitted on Encrypted Storage Devices (ESDs) or via secure data transfer
You will have to formally submit four therapy video recordings over the year: one formative and three summative; the summative recordings are to be submitted at the end of terms 2, 3 and 4. In addition, three formative assessments of therapy sessions will be completed within university group supervision, in terms 2,3 & 4. Summative video recordings should be of those clients you use as your closely supervised clients and link to some of the other course assessments (case reports).
Two additional “live competency assessments” using actors, will be assessed by course supervisors at the beginning and end of the course. These are formative assessments and are intended to assess your training needs, inform supervision and to provide formative feedback for ongoing clinical skills development at the end of the taught course. The outcomes are also used to assess the contribution of the training course to CBT skills development.
To aid understanding of the CTS-R, there will be opportunities to view previous trainees' clinical sessions and feedback as part of the teaching programme, where consent has been given for this purpose.
Guidance on Recording Sessions
In CBT, it is standard practice to record therapy sessions which can be given to the client to listen to between sessions and used for supervision and reflective practice. For the purpose of assessment and supervision, with client consent, video recordings will be used to assess your clinical skills.
You will be expected to submit recordings via secure data transfer as part of the clinical assessment and bring recordings to supervision. It is essential that you obtain the consent of your client for the recording to be used for supervision and/or assessment and submit the consent form with your recording. The consent form also asks whether your client will be willing for the recording to be used in future training. You should consult your workplace supervisor and manager about your Workplace policies on making, transporting, storing and disposing of the recordings in line with Information Governance policies and procedures
You will formally submit four video recordings on via secure data transfer for assessment of clinical sessions (one formative, three summative) over the year.
Recording Equipment
Any service is providing face to face sessions should provide trainees with video recording equipment. Please ensure that the recordings are saved in a file format playable on Windows media player or VLC media player when submitting recordings.
Reflective summaries and self-ratings
Each of the formative and summative assessments of CBT competences via CTS-R submitted/viewed need to be accompanied by a written reflective summary on 1 or 2 themes/issues relevant to the session and a self-rating using the CTS-R. Please see the 'reflective practice' section of the handbook for further guidance and the 'forms for download' section for the relevant paperwork to complete.
Guidance on Formative CBT Competencies Assessments via CTS-R
Within university group supervision - formative assessment of CBT competencies.
Term 2 - the focus of training in term 2 will be working with anxiety disorders and PTSD. Therefore, it is anticipated that you will bring a client, with a presenting problem of an anxiety disorder, or and PTSD as your closely supervised client throughout term 1 and 2 supervision. You will provide a video recording of a full therapy treatment/intervention to be observed within group supervision for formative assessment using the CTS-R and also present your CTS-R self-rating and CTS-R Reflection for formative feedback. It is anticipated that you will obtain a minimum overall mark of 30% for this work.
Term 3 – the focus of training in term 3 will be working with depression. You will bring a client, presenting with an anxiety disorder or post-traumatic stress disorder as your closely supervised case for the first 3 - 4 weeks and then bring a client with depression for the last 6-7 weeks. You will present a video recording of a full therapy treatment/intervention to be observed within group supervision for formative assessment using the CTS-R and also present your CTS-R self-rating and CTS-R Reflection for formative feedback. It is anticipated that you will obtain a minimum overall mark of 40% for this work.
Term 4 - the focus of training in term 4 will be working with complexity/co-morbidity across anxiety and depression. This does not mean that the client brought for close supervision at the university needs to be presenting with complexity/comorbidity. In Term 4, you will continue to bring your ongoing closely supervised clients, presenting with an anxiety disorder or post-traumatic stress disorder or depression. You will bring a 10 – 20 min recording excerpt of a therapy treatment/intervention session to focus on a specific skill/competency to group supervision for formative assessment using the CTS-R. You will also present your full CTS-R self-rating and CTS-R Reflection for formative feedback. It is anticipated that you will obtain a minimum overall mark of 40% for this work.
Guidance on SUMMATIVE CBT Competencies Assessments via CTS-R
The Summative CBT Competencies Assessments (CTS-R & Reflection) must be submitted by the deadlines in term 2 (PYCM039) and term 3 and 4 (PYCM038 and PYCM040). The video recording must be clearly audible and be of a complete (unedited) therapy treatment/intervention session (50 – 60mins, unless extended time agreed and in accordance with relevant NICE Guidance, e.g. PTSD and Social Anxiety Disorder). When recording face to face sessions, both therapist and client must be front facing and clearly visible. Your recording must be submitted along with a completed front cover sheet which includes your own self-ratings of CBT competencies and a CTS-R Reflection of the recording presented. You should also include the formulation and completed consent to record form.
You MUST achieve a minimum CTS-R mark of 50% which corresponds to a raw score of 36 and above. However, you MUST also achieve a rating of at least 2 on EVERY item in order to pass. Your CTS-R Reflection must also be passed as satisfactory.
Anxiety Module (PYCM039) - you will submit a video recording demonstrating CBT competencies for anxiety, or PTSD, term 2. This submission should be of a session from the treatment phase (session 3- 4 onwards) of your work with the same client that you have written up for your Anxiety Case Report and be the same client you have brought to University supervision during term 2 as your closely supervised client.
Depression Module (PYCM038) – you will submit a video recording demonstrating CBT competencies for depression at the end of term 3. This submission should be of a session from the treatment phase (session 3- 4 onwards) of your work with the same client that you have written up for your Depression Case Report and be the same client you have brought to University supervision during term 3 as your closely supervised client.
Clinical Practice Module (PYCM040) - The end of term 4 submission of a session video recording demonstrating CBT competencies should be of the client you have brought to University supervision during term 3 as your closely supervised client with a different anxiety disorder presentation than the term 2 assessment. This submission should be of a session from the treatment phase (session 3- 4 onwards) of your clinical practice.
Introduction
This is a scale for measuring therapist competence in Cognitive Therapy and is based on the original Cognitive Therapy Scales (CTS. Young & Beck. 1980. 1988). The CTS-R was developed jointly by clinicians and researchers at the Newcastle Cognitive and Behavioural Therapies Centre, and the University of Newcastle upon Tyne, UK.
The CTS-R contains 12 items, in contrast to earlier versions of the CTS which contained either 13 (Young & Beck, 1980) or 11 (Young & Beck, 1988). The development of the revised scale, together with the psychometric properties, is described in the appendices.
Table 1: The CTS-R Items
| General items | Cognitive therapy specific items |
|---|---|
|
Item 1: Agenda Setting & Adherence* Item 2: Feedback |
Item 1: Agenda Setting & Adherence* Item 6: Eliciting Appropriate Emotional Expression ** Item 7: Eliciting Key Cognitions Item 8: Eliciting and Planning Behaviours** Item 9: Guided Discovery Item 10: Conceptual Integration Item 11: Application of Change Methods Item 12: Homework Setting |
* Item 1 can be regarded as both a general and CT item.
** Items 6 and 8 are new items developed for the scale.
Theoretical Bases of the Scale
Two frameworks underpin the revised scale, the Cognitive Cycle and the Dreyfus Scale of Competence (Dreyfus, 1989).
The Cognitive Cycle: The cognitive cycle represented in Figure 1 demonstrates how the CTS-R items address specific cognitive features. At the heart of the scale, as in therapy, is the conceptualization. In order to move the patient from a dysfunctional cycle, dominated by a dysfunctional conceptualization, the therapist must address the four features highlighted in the outer ring of the circle: thoughts, feelings, physiology and behaviour/planning. In terms of therapeutic competence, the therapist's must be skilled at encouraging the patient to move around the points of the cycle, using the Cognitive Specific items (Items 6-12) to address the features. To facilitate the smooth movement around the cycle, the therapist must also demonstrate competence in areas assessed by the remaining items 1-5 (agenda and adherence, feedback, collaboration, pacing, interpersonal effectiveness).
Figure 1: The relationship between the CTS-R items and the Cognitive Cycle.
Items facilitating movement around circle
- Agenda Setting
- Feedback
- Collaboration
- Pacing & Efficient use of time
- Interpersonal Effectiveness
Dreyfus Model of Competence: The Dreyfus Model has also been incorporated within the CTS-R. It is designed to assess the level of competence shown by the therapist (see Table 2). In the original Dreyfus scale there are five levels, to this we added a further level to denote 'incompetence', as outlined below.
Table 2: Adapted Dreyfus level of Competence
Incompetent - The therapist commits errors and displays poor and unacceptable behaviour, leading to negative therapeutic consequences.
Novice - At this level the therapist displays a rigid adherence to taught rules and is unable to take account of situational factors. He/she is not yet showing any discretionary judgement.
Advanced Beginner - The therapist treats all aspects of the task separately and gives equal importance to them. There is evidence of situational perspective and discretionary judgement
Competent - The therapist is able to see the tasks linked within a conceptual framework. He/she makes plans within this framework and uses standardised and routinised procedures.
Proficient - The therapist sees the patient's problems holistically, prioritises tasks and is able to make quick decisions. The therapist is clearly skilled and able.
Expert - The therapist no longer uses rules, guidelines or maxims. He/she has deep tacit understanding of the issues and is able to use novel problem-solving techniques. The skills are demonstrated even in the face of difficulties (e.g. excessive avoidance).
This model has been incorporated within the scoring system as demonstrated in the scoring layout below.
Scoring system
A detailed explanation of the scoring system is provided below. As you can see. each item is rated on a Likert scale, ranging from 0-6. Each level being defined in detail to conform to the levels of competence (see Table 2).
Example of the scoring layout:
Key features: this is an operationalised description of the item (see examples within the CTS-R).
Mark with an 'X' on the vertical line, using whole and half numbers, the level to which you think the therapist has fulfilled the key features. The descriptive features on the right are designed to guide your decision.
Scoring system example.
Please note that the top marks (ie. near the 'expert' end of the continuum) are reserved for those therapists demonstrating highly effective skills, particularly in the face of difficulties (ie. highly aggressive or avoidant patients; high levels of emotional discharge from the patients; and various situational factors).
Maximum score on the scale is 72 (12x 6). At the Newcastle Cognitive Therapy Centre we set a minimum competence standard of 36, which would be an average of 3 marks per item.
Item 1- Agenda Setting and Adherence
Introduction
The agenda helps ensure that the most important issues are addressed in an efficient manner. Therapist and patient must establish these issues jointly. The agenda should review items from the previous session(s), in particular the homework assignment, and include one or two items for the session. Once set, it should be appropriately adhered to. However, if changes are necessary, because of an important new issue arising, the deviation from the agenda should be made explicit.
The key features of the 'agenda' is outlined in the CTS-R Rating Scale as follows:
| Key features: To address adequately topics that have been agreed and set in an appropriate way. This involves the setting of discrete and realistic targets collaboratively. The format for setting the agenda may vary according to the stage of therapy - see manual. Three features need to be considered when scoring this item:
NB: Agenda setting requires collaboration and credit for this should be given here, and here alone. Collaboration occurring at any other phase of the session should be scored under Item 3 (Collaboration). |
Short-term cognitive therapy requires that the important issues are discussed sensitively but managed in a business-like way. In order to cover a lot of material adequately in a relatively short space of time, specific and realistic targets need to be set in a collaborative manner, and adhered to appropriately. Indeed, it is of limited use to set a good agenda and then not be guided by it.
On setting the agenda the therapist must ensure the items are appropriate. They should be suitable for the stage of therapy, amenable to a CT rationale, consistent with the formulation, and conceived to take the therapy forward. In addition, the items should be clear and discrete. If the items are too vague, this may lead to confusion and also result in divergent and tangential material being discussed. It is important to note, however, that the therapist must be aware not to let the patient go into too much detail about anyone item at this stage, as this will disrupt the agenda setting process. The therapist must be careful not to include too many items, as this may lead to either important items being missed or the therapy being rushed.
The list of items should include material from both the patient and therapist. A discussion of the homework which was set previously should be a 'standing' item. Even when no homework was set in the previous session (for whatever reason), the value of such assignments should be discussed in order to restate the importance of this aspect of therapy. Unless this is done the patient may come to think that there is no need to complete the assignment carefully.
Part of socialising the patient to CT is to establish an expectation that he/she will need to come to each session having thought through the key topics for that day's therapeutic work.
Following the setting of the agenda, the patient should be asked to prioritise his/her list of items. The prioritisation permits the therapist to plan the session and allot appropriate time for the material. Efficient prioritising facilitates the pacing of the therapy.
CHECKLIST: QUESTIONS FOR RATERS TO ASK THEMSELVES:
- Did the therapist set an agenda with clear, discrete, and realistic goals - and adhere to it?
- Can you identify at least two specific agenda items?
- Was the patient encouraged to participate in setting the agenda?
- Do you think the patient clearly understood what the therapy was going to cover?
- Did the agenda seem appropriate?
- Were the items prioritised?
- Did you hear any of the following:
- What would you like to get from today's session?
- What is the most important thing to cover today? ... Are there any other things to include?
- Is there anything that has been troubling you this week, which might help to illustrate your problems?
- You have mentioned X, Y and Z. Which of these would you like to talk about first?
- If we did discuss this item, how would it help take the therapy forward?
Item 2 - Feedback
Introduction
The therapist should both provide and elicit feedback throughout each session. The therapist's feedback should occur at regular intervals and is particularly important at the end of the therapy session. This feedback helps to focus the patient on the main therapeutic issues, and assists in reducing vague or amorphous issues into manageable units. It also helps both the therapist and the patient to determine whether they have a shared understanding of the problems and concerns.
Eliciting feedback ensures that the patient understands the therapist's interventions. formulations and lines of reasoning. It also allows the individual to express positive and negative reactions regarding the therapy.
The key features of 'feedback' is outlined in the CTS-R Rating Scale as follows:
| Key features: The patient's and therapist's understanding of key issues should be helped through the use of two-way feedback. The two major forms of feeding back information are through general summary and chunking of important units of information. The use of appropriate feedback helps both the therapist to understand the patient's situation, and the patient to synthesise material enabling him/her to gain major insight and make therapeutic shifts. It also helps to keep the patient focused. Three features need to be considered when scoring this item:
|
This item stresses the importance of two-way feedback. By 'summarising' and 'chunking' information at regular intervals, the therapist can emphasise the major features, synthesise new material and highlight issues that require further clarification. By eliciting the patient's feedback (thoughts and feelings) regarding the therapy, the therapist can check the patient's attitude, knowledge base and understanding.
Chunking information and eliciting feedback should occur frequently. On occasions, when either particularly important or confusing material is being discussed, the feedback should occur after each major point; this can also help 'contain' distressing issues. During normal short-term CT, the two-way feedback should occur at least every 10 minutes.
Major summaries should occur at the beginning and end of each session, to help reinforce and consolidate therapeutic material.
It is important that the feedback be appropriate. For example, when providing feedback the therapist must choose the salient material presented to him her, and then summarise these features in a way that both clarifies and highlights key issues. This form of summarising and feeding back is the foundation for many forms of cognitive techniques (eg. Socratic questioning). When eliciting feedback. the therapist should be aware that patients (especially people suffering from depression) often indicate understanding simply out of compliance. Hence. it is vital that the therapist explores the patient's understanding and attitude towards the therapy carefully.
The manner in which the feedback is elicited and delivered is also important. For example. the therapist should be sensitive to negative and covert reactions expressed both verbally and non-verbally by the patient and should also ask for the patient's thoughts when such clues are noticed. Whenever appropriate the therapist should ask the patient either for suggestions about how to proceed. or to choose among alternative courses of action.
When giving feedback the therapist should deliver it in a manner that is constructive and helps to move the therapy forward. This will involve anticipation of how the information may be received (eg. perceived as criticism).
CHECKLIST: QUESTIONS FQR RATERS TO ASK THEMSELVES:
- Do you think the feedback was appropriate? ... Sufficiently frequent?
- Did the therapist chunk the salient pieces of information to provide a platform for new insight?
- Was the patient encouraged to provide feedback throughout the session?
- Do you think that the feedback was used effectively in helping the patient's understanding?
- Did you hear any of the following:
- Could you tell me the three most important issues we've discussed today?
- Just to summarise, at the beginning of the session we spoke about X and the effect it had on your feelings. Then we discussed Y, etc. etc.
- I think I have understood what you just said, let me see if I can repeat back the main points.
Item 3 - Collaboration
Introduction
Good therapeutic teamwork is a fundamental feature of cognitive therapy. Collaboration should be consistent throughout the session, although at times didactic approaches may be necessary (eg. educating the patient about the physical effects of anxiety).
The key features of 'collaboration' is outlined in the CTS-R Rating Scale as follows:
Key features: The patient should be encouraged to be active in the session. There must be clear evidence of productive teamwork, with the therapist skilfully encouraging the patient to participate fully (e.g. through questioning techniques, shared problem solving and decision making) and take responsibility. However, the therapist must not allow the patient to ramble in an unstructured way. Three features need to be considered: the therapist style should encourage effective teamwork through his/her use of:
NB: Questioning is a central feature with regard to this item, but questions designed to facilitate reflections and self discovery should be scored under Item 9 (Guided Discovery). |
As mentioned above, collaboration will be used during Agenda Setting (Item 1) and should be credited accordingly within this item. Hence, credit on this item should only be given for evidence of collaboration that occurs outwith Agenda Setting.
The therapist should adopt a style that promotes an egalitarian relationship, whereby he/she and the patient work actively towards shared goals. This is achieved by the development of a 'teamwork' approach. Hence the therapist should avoid being overly directive, too intellectual, controlling or passive.
The therapist needs to strike a balance between being structured on the one hand and on the other allowing the patient to make choices and take responsibility. In order to achieve a good therapeutic alliance, the therapist must assess the patient's needs, and particularly his/her preferred modes of learning. For example, Beck (1983) suggests that individuals who display sociotropic traits respond better to a warm supportive therapeutic relationships, while those with autonomous traits prefer to take a high level of responsibility within the therapy and respond better to a more task-oriented approach.
Good Collaboration will also involve striking a balance between the verbal and non-verbal features. For example, deciding when to talk and when to listen; when to confront and when to back-off; when to offer suggestions and when to wait for the patient to devise his/her own.
Another important element of Collaboration is for the therapist to be open about the process and status of therapy. This will include the therapist explaining the rationale for interventions, admitting confusion; sharing summaries both verbally and in writing.
CHECKLIST: QUESTIONS FOR RATERS TO ASK THEMSELVES:
- Was the patient encouraged to participate fully?
- Was the therapist able to establish a collaborative relationship?
- Did the therapist give the patient sufficient space and time to think?
- Was the therapist overly directive or too controlling?
- Did you hear any of the following:
- How might we test that out?
- What are the problems of behaving that way?
- Perhaps we could work out an alternative way of looking at this issue.
- Before setting this behavioural task, let's examine the potential obstacles which might prevent us learning anything from it.
- That's a difficult one, so let's put our heads together and try and think it through.
- Does this sound reasonable to you?
Item 4 - Pacing and Efficient Use of Time
Introduction
The therapist should make optimal use of the time in accordance with items set in the agenda. He/she must maintain sufficient control, limit discussion of peripheral issues, interrupt unproductive discussion, - and pace the session appropriately. Nevertheless, the therapist should avoid rushing crucial features of the session.
The key features of 'Pacing and efficient use of time' is outlined in the CTS-R Rating Scale as follows:
Key features: The session should be well 'time managed' in relation to the agenda, with the session flowing smoothly through discrete start, middle, and concluding phases. The work must be paced well in relation to the patient's needs, and while important issues need to be followed, unproductive digressions should be dealt with smoothly. The session should not go over time, without good reason. Three features need to be considered:
|
The session should be well time managed, such that it is neither too slow nor too quick. For example, the therapist may unwittingly belabour a point after the patient has already grasped the message, or may gather much more data than is necessary before formulating a strategy for change. In these cases, the sessions can seem painfully slow and inefficient. On the other hand, the therapist may switch from topic to topic too rapidly, thus not allowing the patient to integrate the new material sufficiently. The therapist may also intervene before having gathered enough data to conceptualise the problem. In summary, if the therapy is conducted too slowly or too quickly, it may impede therapeutic change and could de-motivate the patient.
The pacing of the material should always be accommodated to the patient's needs and speed of learning. For example, when there is evidence of difficulties (eg. emotional or cognitive difficulties), more time and attention may need to be given. In such circumstances the agenda items may be shuffled or adapted accordingly. In some extreme circumstances (eg. disclosure of suicidal thoughts), the structure and pacing of the session will need to change drastically in accordance with the needs of the situation.
The therapy should move through discrete phases. At the start, there should be a structured agenda. Then the agreed plan of the session should be handled efficiently during the main phase.
It is important that the therapist maintains an overview of the session to allow correct pacing throughout. This may involve the therapist politely interrupting peripheral discussion and directing the patient back to the agenda.
A well paced session should not need to exceed the time allocated for the period and should cover the items set in the agreed agenda. It will also allow sufficient time for the homework task to be set appropriately, and not be unduly rushed.
CHECKLIST: QUESTIONS FQR RATERS TO ASK THEMSELVES:
- Was the therapist able to recognise the patient's need and adapt the session accordingly?
- Was there any time during the session when the session moved too slowly/quickly (eg. agenda setting phase)?
- Do you think the session flowed well overall?
- Was the therapist able to avoid unproductive digressions?
- Was there sufficient time left for the homework assignment?
- Was the pacing of the session adapted well to the needs of the patient?
- Did the patient appear rushed?
- Did you hear any of the following:
- How much time should we spend on that item?
- Do you mind stopping a second, you've given me too much information too quickly. Let's try to look at the major points you're trying to make.
- We've strayed off the topic a little. I feel it is important to try to focus on the chief issues you raised.
- Now we have 20 minutes left before the end of the session. Is there anything you feel we must cover before the end - keeping in mind that we will also need to set the homework assignment?
Item 5 - Interpersonal Effectiveness
Introduction
The ability of the therapist to form a good relationship with the patient is deemed crucial to the therapy. Indeed, in order for the patient to be able to disclose difficult material, there must be both trust and confidence in the therapist. Rogers suggests that the non-specific factors of 'empathy, genuineness and warmth' are key features of effective therapy.
The key features of 'Interpersonal Effectiveness' is outlined in the CTS-R Rating Scale as follows:
Key features: The patient is put at ease by the therapist's verbal and non-verbal (e.g. listening skills) behaviour. The patient should feel that the core conditions (ie. warmth, genuineness, empathy and understanding) are present. However, it is important to keep professional boundaries. In situations where the therapist is extremely interpersonally effective, he/she is creative, insightful and inspirational. Three features need to be considered:
|
In order that the appropriate levels of the three features are conveyed, careful judgement is required from the therapist. Personal and contextual needs must be taken into account. For example, towards the end of therapy lower levels of warmth may be used, as compared to the beginning, in order to promote patient disengagement.
Empathy concerns the therapist's ability to make the patient aware that their difficulties are recognised and understood on both an emotional and cognitive level. The therapist needs to show that he/she shares the patient's feelings imaginatively. For example, the promotion of a shared-value system between therapist and patient will help to enhance this aspect of the relationship. The therapist should avoid appearing distant, aloof or critical.
A good therapist should adopt a genuine and straightforward therapeutic style. A sincere and open style will promote a trusting, collaborative working relationship. The therapist should avoid appearing condescending or patronising.
It is also important for the therapist to convey warmth and concern through both his/her verbal and non-verbal behaviour. The therapist should avoid being critical, disapproving, impatient or cold. He/she should convey an attitude of acceptance of the person, but not of course with respect to the style of thinking.
It is important to highlight that appropriate use of humour can often help to establish and maintain a good therapeutic relationship.
CHECKLIST:QUESTIONS FOR RATERS TO ASK THEMSELVES:
- Did you consider the relationship was positive?
- Was the therapist displaying appropriate empathy, understanding, warmth and genuineness?
- Did he/she appear appropriately genuine, helping to facilitate therapeutic trust?
- Do you think he/she showed acceptance and liking of the individual, while remaining within professional boundaries?
- Did the therapist appear confident?
- Did you hear any of the following:
- I understand that X was difficult for you to do
- Shared laughter
- This must have felt awful for you
Item 6 - Eliciting Appropriate Emotional Expression
Introduction
The ability of the therapist to deal effectively with the emotional content of the therapy session is a crucial feature of therapy. The therapist should be able to increase or reduce the emotional ambience of a session through his her verbal and non-verbal behaviour. The therapist should then be able to use the patient's emotions to promote therapeutic change. The current item reflects the degree to which the therapist is able to create the circumstances through which emotional change and expression can be elicited and then used effectively.
Key features: The therapist facilitates the processing of appropriate levels of emotion by the patient. Emotional levels that are too high or too low are likely to interfere with therapy. The therapist must also be able to deal effectively with emotional issues which interfere with effective change (eg. hostility, anxiety, excessive anger). Effective facilitation will enable the patient to access and express his/her emotions in a way that facilitates change. Three features need to be considered:
|
Cognitive therapy requires both cognitive and emotional shift. In order to produce emotional change the therapist must first facilitate the patient to express themselves on an emotional level. The therapist should ensure that emotions associated with a particular situation or cognition are elicited and assessed for intensity. The therapist must also be able to assess the emotional shift within a session and work with it accordingly; increasing and decreasing the level of emotionality as appropriate (see Figure 6.1).
There is an optimal level of emotional affect required to motivate a person to change constructively. Too little emotional energy (ie. apathy, lack of motivation, avoidance) will be insufficient to create change. In these cases the therapist must first be able to stimulate the patient (through verbal and non-verbal behaviour) to become an active participant in the therapeutic process.
On the other hand too much emotion (ie. anger, despair, fear, etc.) will interfere with therapy. The therapist should be able to contain the energy. or use or dissipate it, in order that it no longer serves as an obstacle to effective change.
Figure 6.1: Curve of energy levels for optimal learning
A skilled therapist will also recognise inconsistency between the emotional and cognitive content, and explore such discrepancies accordingly. For example, if a patient expresses no distressful emotion when talking about some unpleasant event, careful questioning will help the patient access his/her associated emotions.
CHECKLIST: QUESTIONS FOR RATERS TO ASK THEMSELVES:
- Did the therapist pay sufficient attention to the person's emotions?
- Did the therapist help the patient to differentiate between different emotions?
- Did the therapist raise emotional topics in a sensitive manner?
- Was there an optimal level of emotional arousal to promote change?
- Did the therapist's activity serve to motivate the patient appropriately?
- Did the therapist prepare the patient to work on his/her emotions?
- Was the therapist able to contain any emotional outbursts?
- Did you hear any of the following:
- How did that make you feel?
- You seem very angry today? Am I right?
- If you tried to do that, how would it make you feel?
- You appear to be fearful of talking about that subject, but I'm going to have to press you a little more.
- Did you feel anything else than sadness?
- You are relating very distressing events, and you are smiling. How do you understand this?
Item 7 - Eliciting Key Cognitions
Introduction
Cognitive therapy stresses the role of cognitions and the emotions associated with them in the genesis and maintenance of a range of psychiatric disorders. The current feature addresses the ability of the therapist to elicit important cognitions in an effective manner.
It is important to note that there are a number of techniques used frequently to elicit key cognitions, for example thought monitoring (eg. thought eliciting diaries) and downward arrowing techniques. Such methods should be scored under this item rather than Item 11 (Application of Change Methods). The latter item is concerned with change techniques.
The key features of 'Eliciting Key Cognitions' is outlined in the CTS-R Rating Scale as follows:
| Key features: To help the patient gain access to his/her cognitions (thoughts, assumptions and beliefs) and to understand the relationship between these and their distressing emotions. This can be done though the use of questioning, diaries and monitoring procedures. Three features need to be considered:
|
A therapist should be able to identify and elicit those thoughts, images and beliefs which are fundamental to the patient's distress (ie. the key cognitions). Key cognitions often take the form of negative automatic self-statements or beliefs relating to the self and the world that either drive or maintain negative emotions.
In the case of depression, such negative automatic thoughts (NATs) might be:
Other types of key cognitions are dysfunctional core beliefs (core schemata, Early Maladaptive Schemata). These are rigid, inflexible and dysfunctional self-beliefs which are not open to the 'normal' corrective processes of logical thinking. These can be expressed through basic assumptions and rules (If ... then; I should ...; people should...).
The negative automatic thoughts, basic assumptions, rules and core beliefs often exist in the face of overwhelming contradictory evidence (eg. The eminent professor who thinks she is worthless). As part of the assessment, it is also important for the therapist to determine the different forms of cognitive biases being used to support the patient's thinking. For example, the patient may be engaging in 'minimising the positive': reducing the frequency or impact of good events, perhaps even focusing on the negative side of such events (eg. "Now that I've got a new job, I’ll have to get up early") OR, 'catastrophising': exaggerating the potential negative impact of an occurrence out of all reasonable proportions (eg. "Mark didn't call last night, I don't think he likes me any more"). Other cognitive biases include: overgeneralising, black and white (absolute) thinking, etc.
On certain occasions the patient may display a great deal of emotion (cry, shake, etc.) while discussing issues. At such times, the patient's thinking needs to be checked-out as he/she may be experiencing dysfunctional thoughts at that moment (such thoughts are termed 'hot cognitions'). During such an episode, the therapist must exercise a great deal of empathy and skill when eliciting these cognitions.
The therapist should also be able to elicit the key cognitions, when they are not immediately apparent The therapist needs to use his her professional judgement in determining which are the 'key' cognitions, taking into account both the needs of the patient and the stage of therapy. For example, during the first few sessions it is not usually appropriate to elicit and tackle core beliefs, because the patient will not be sufficiently socialised to the therapy for effective work to be done.
CHECKLIST: QUESTIONS FOR RATERS TO ASK THEMSELVES:
- Was the therapist able to identify and elicit the appropriate cognitions and biases?
- Was the therapist able to access and work with key cognitions?
- Was the therapist able to identify thinking biases and elicit hot cognitions?
- Were the cognitions elicited well?
- Does the therapist adequately demonstrate to the patient how to identify key cognitions and biases?
- Did you hear any of the following:
- What was going through your mind at the time?
- Did you make anything of that?
- What did you say to yourself when ...?
- There seems to be a rule there that you apply to yourself. Do you see what it is?
- A word that comes up often in these records is “weak". Is this how you see yourself in general?
- If you didn't finish your work on time, what would this say about you?
Item 8 - Eliciting and Planning Behaviours
Introduction
Behavioural problems are observed frequently in psychiatric disorders. They take numerous forms. including withdrawal, avoidance, compulsions and various types of safety behaviours. As such, it is important that the therapist elicits the roles these behavioural features play in the maintenance of the patient's problems. In addition. the therapist needs to elicit and develop practical plans with the patient in order that effective change takes place (eg. the where, what, when, and how of a desensitization programme).
Both of these features are addressed in this item.
|
Key features: To help the patient gain insight into the effect of his/her behaviours with respect to the problems. This can be done through the use of questioning, diaries and monitoring procedures. The therapist works with the patient to plan strategies either to overcome or disrupt dysfunctional behavioural patterns.
NB: This item is concerned with the general work done with eliciting behaviours and plans. If any specific cognitive or behavioural change methods are used. they should be scored under item 11 (Application of change methods). |
It is important to examine the role behaviours have in triggering and maintaining the patient's disorders. Behaviours often reinforce both negative thoughts and feelings. For example, the typical avoidance observed in social phobia prevents the person overcoming his/her fear, and obtaining the skills necessary to engage in social interactions.
Such activities can be termed “safety behaviours" as patients employ them as a means of reducing their levels of distress (eg. avoidance and escape reactions). However, safety behaviours can often serve to unwittingly maintain a person's problems, ensuring that the dysfunctional cycles are preserved. On occasions the patient might react to difficulties by over-compensating in some manner (eg. becoming aggressive when feeling vulnerable); this pattern clearly ought to be elicited and dealt with. The eliciting process requires skill, as the patient needs to be made aware of the helpful and unhelpful sides to the various courses of action. The process thus requires the therapist to use effective, flexible and appropriate methods to motivate the patient to behave differently in the future.
Part of the process of producing effective behavioural change is the development of plans which help to test out hypotheses and break unhelpful patterns of behaviour. For example, when setting a behavioural task, the therapist should get the patient to:
- think through the relevance of the assignment
- be confident in his/her ability to perform it, and be sufficiently motivated
- check through anticipated level of arousal
- plan what needs to be done carefully, and be cognisant of potential obstacles
- practice the behaviour
- be able to relate either success or failure to a change in perspective
In planning the task, relevant questions should be asked of the person's concepts, cognitions, affective and physiological states, and behavioural repertoire. See Figure 8.1 below.
Figure 8.1: Examples of questions used when planning a behavioural intervention
A thorough planning exercise would address the impact of the behaviour in terms of all aspects of the generic cognitive cycle, including motivation for change and potential obstacles.
CHECKLIST: QUESTIONS FOR RATERS TO ASK THEMSELVES:
- Did the therapist examine adequately the role of behavioural features played in the triggering and maintenance of the patient's problems?'
- Did the therapist help the patient discover the impact of his/her behaviours in terms of cognitive rationale?
- Where the pros and cons of behavioural aspects examined?
- Did the therapist help the patient plan and develop useful change strategies?
- Did you hear any of the questions highlighted in Figure 8.1. see above.
Item 9 - Guided Discovery
Introduction
Guided discovery is a form of presentation and questioning which assists the patient to gain new perspectives for himself/herself without the use of debate or lecturing. It is used throughout the sessions in order to help promote the patient to gain understanding. It is based on the principles of socratic dialogue, whereby a questioning style is used. to promote discovery, to explore concepts, synthesise ideas and develop hypotheses regarding the patient's problems and experiences.
The key features of 'Guided Discovery' is outlined in the CTS-R Rating Scale as follows:
| Key features: The patient should be helped to develop hypotheses regarding his/her current situation and to generate potential solutions for him/herself. The patient is helped to develop a range of perspectives regarding his/her experience. Effective guided discovery will create doubt where previously there was certainty, thus providing the opportunity for re-evaluation and new learning to occur. Two features need to be considered:
|
It has been observed that patients are more likely to adopt new perspectives, if they perceive they have been able to come to such views and conclusions for themselves. Hence, rather than adopting a debating stance, the therapist should use a questioning style to engage the patient in a problem solving process.
Skilfully phrased questions, which are presented in a clear manner, can help to highlight either links or discrepancies in the patient's thinking. In order to accommodate the new information or learning, new insight is often achieved. Padesky (1993) emphasises that the aim of questioning is not to 'change minds' through logic, but to engage the patient in a socratic dialogue. Within this dialogue the patient can arrive at new perspectives and solutions for themselves.
The therapist's questioning technique should reveal a constant flow of inquiry from concrete and specific ("Does your mood drop every time you argue with your mother?”) to abstract ("Do you always feel this way when someone is shouting at you?”) and back again (“What thoughts were going through your head when it was your mother shouting?"). Good questions are those asked in the spirit of inquiry, while bad ones are those which lead the patient to a predetermined conclusion.
The techniques may also permit the patient to make both lateral and vertical linkages. The lateral links are those day to day features of the patient's life which produce and maintain his/her difficulties (ie. the NATs, dysfunctional behaviours, moods and physical sensations). The vertical links are the historical patterns and cycles, which manifestly relate to the patient's current problems (ie. childhood issues, parenting, relationship difficulties, work issues, etc.).
The questions posed should not be way-beyond the patient's current level of understanding, as this is unlikely to promote effective change. Rather they should be phrased within, or just outside, the patient's current understanding in order that he/she can make realistic attempts to answer them. The product of attempting to deal with such intelligently phrased question is likely to be new discoveries.
The therapists should appear both inquisitive and sensitive without coming across as patronising.
CHECKLIST: OUESTIONS FOR RATERS TO ASK THEMSELVES:
- Has the therapist used appropriate questions?
- Does the manner in which the questions are asked facilitate the patient's understanding?
- Did the questions lead to or promote change?
- Did you hear any of the following:
- I wonder whether there are any other times in your life when you felt the same way?
- You have this dreadful image when you're with both John and Paul, but you never have it with Peter. Can you think of a reason for this?
- If you were not depressed, how might you think differently about this situation?
- How does this relate to what you told me earlier - that you never get anything right?
- What is the common link between X and Y?
Item 10 - Conceptual Integration
Introduction
Conceptualisation concerns the provision of an appropriate knowledge base that promotes understanding and facilitates therapeutic change. It encompasses both the cognitive therapy rationale and the cognitive formulation. Through the conceptualisation the patient will gain an understanding of the cognitive rationale of his/her disorder, its underlying and maintaining features, and relevant triggers. Importantly, the patient should also gain an understanding of the relative efficacy of the coping strategies currently being used in order to deal with the problem.
The conceptualisation process involves initially socialising the patient to the therapeutic rationale (ie. establishing the links between "thoughts → feelings → behaviours"). This rationale (ie. the generic CT model) is presented in Figure 10.1. Its specific format will vary with respect to the different disorders.
Figure 10.1: The generic CT model
After the initial assessment phase, the process involves the development of an appropriate understanding of the problem. This is termed formulation, and is a personalised account of the disorder in terms of both its genesis and maintaining features. The formulation involves establishing the lateral (ie. situational and maintaining features) and vertical (ie. historical) linkages underpinning the disorder. Figure 10.2 presents an integrated formulation, using both vertical and lateral linkages.
Figure 10.2: Integrated Formulation
Following the formulation, the patient must acquire the knowledge of what needs to be changed and the most appropriate strategies for change (ie. change mechanisms). When working effectively, both the therapist and patient will have a shared theoretical understanding of the aims, model and current status of the therapy with respect to the therapeutic goals.
The key features of 'conceptualisation' is outlined in the CTS-R Rating Scale as follows:
| Key features: The patient should be helped to gain an appreciation of the history, triggers and maintaining features of his/her problem in order to bring about change in the present and future. The therapist should help the patient to gain an understanding of how his/her perceptions and interpretations, beliefs, attitudes and rules relate to his/her problem. A good conceptualisation will examine previous cognitions and coping strategies as well as current ones. This theory-based understanding should be well integrated and used to guide the therapy forward. Two features need to be considered:
|
Conceptualising is one of the key processes of therapy through which change takes place. It provides the theoretical overview of the work. Its absence can lead to disjointed therapy, which might prevent major insight being gained by the patient. When it is not appropriately integrated within therapy, the work may lose its focus and only consist of a set of unrelated techniques.
In order for effective therapy to occur the conceptualisation must be appropriate. To arrive at an appropriate cognitive rationale a thorough assessment needs to take place, in which both therapist and patient collect information to increase their understanding of the problem. Through this data-gathering process the patient learns to monitor the important features of his/her disorder (NATs, feelings, behaviours, safety behaviours, cognitive biases, etc.), and thereby gain further insight To instigate this process effectively, the therapist must have a good theoretical understanding of generic cognitive therapy and the specifics of the patient's disorder (ie. the cognitive models of depression, panic, OCD, PTSD, etc.).
During this period, patients learn to break down situations using the rationale. In essence, they begin to become their own therapist. This process is often facilitated greatly through the use of suitable written material. Typically the therapist will illustrate relationships via diagrams or through the use of examples, stories and/or metaphors. If not performed adequately, the patient can feel misunderstood and alienated. He/she may become less active both in an out of sessions.
A good collaborative relationship is usually essential in developing a comprehensive formulation. The therapist must also be sensitive, particularly when working at the level of core beliefs. It is important to remember, however. that these features should be rated under the relevant items (eg. Collaboration & Interpersonal Effectiveness respectively).
One of the main purposes of establishing the CT rationale is to socialise the patient to the model and generate evidence towards the formulation. The appropriately constructed formulation should be able to explain most of the features of the patient’s disorders (historical and present, including: fears, vulnerabilities, avoidance, maintenance and compensation strategies, effective and dysfunctional coping strategies, etc.). The ultimate aim of the formulation is to arrive at an agreed set of key core beliefs which, based on empirical evidence, make a major contribution to the patient's understanding of his/her current difficulties. Thus the formulation provides the foundation for change. This shared 'frame of reference' then leads on to the choice of treatment techniques that help inform potential change mechanisms.
A good conceptualisation will provide an awareness of effective and dysfunctional cycles of thoughts ↔ emotions ↔ behaviour and thereby suggest potential mechanisms of change.
It is important to note that the patient's self-conceptualisation will not be entirely negative and dysfunctional. Therefore it is vital, when helping to define him/herself, that the therapist highlights the patient's strengths too. This more balanced conceptualisation, may also help clarify areas that could be used effectively in promoting change.
CHECKLIST: QUESTIONS FOR RATERS TO ASK THEMSELVES:
- Has the therapist socialised the patient to the CT rationale?
- Does the therapist demonstrate a good understanding of generic CT?
- Does the therapist demonstrate a good understanding of the CT rationale for the specific disorder?
- Does the patient have an adequate CT understanding of the problem?
- If you asked the patient about his her problems, would he/she be able to produce a working conceptualisation that was broadly consistent with a CT perspective?
- Has the conceptualisation been truly integrated (ie. has it been used to guide the therapy)?
- Did you hear any of the following:
- Let's see how the various things we have talked about hold together.
- What we have done so far is look at the way your thoughts affect the way you feel and what you do. It would be useful for us today to look at some general rules and attitudes that are contained in these thoughts. The reason for doing this is for us to try to understand where they come from. Is this OK with you?
- Do you remember anybody saying this to you: "You are no good"?
- Let's look at times in your life when you have been depressed before.
- Are there times in your life when you have felt good about yourself?
- Does this way of looking at your depression make sense to you?
Item 11 - Application of Change Methods
Introduction
Change methodologies are cognitive and behavioural strategies employed by the therapist which are consistent with the cognitive rationale and/or formulation and designed to promote therapeutic change. The potency of the techniques will depend upon whether they are applied at the appropriate stage in therapy, and the degree to which they are implemented skilfully. It is important to note that during some sessions it may not be appropriate to use a wide range of methods; a rater should take this into account when scoring this item. It is important to note that certain methodologies are rated elsewhere (eg. Eliciting Key Cognitions - Item 7 and Guided Discovery - Item 9), and therefore should not be rated again here.
The key features of 'Application of change methods' is outlined in the CTS-R Rating Scale as follows:
| Key features: Therapist skilfully uses, and helps the patient to use, appropriate cognitive and behavioural techniques in line with the formulation. The therapist helps the patient devise appropriate cognitive methods to evaluate the key cognitions associated with distressing emotions, leading to major new perspectives and shifts in emotions. The therapist also helps the patient to apply behavioural techniques in line with the formulation. The therapist helps the patient to identify potential difficulties and think through the cognitive rationales for performing the tasks. The methods provide useful ways for the patient to test-out cognitions practically and gain experience in dealing with high levels of emotion. The methods also allow the therapist to obtain feedback regarding the patient's level of understanding of prospective practical assignments (ie. by the patient performing the task in-session). Two features need to be considered:
NB: This item is not concerned with accessing or identifying thoughts, rather with their re-evaluation. |
In deciding the appropriateness of a method it is important to determine whether the technique is a coherent strategy for change, following logically from the patient's formulation.
Clinical judgement is required in assessing the degree of skill with which a particular methodology is applied. This feature goes beyond mere adherence (ie. the preciseness with which a technique is applied). Indeed, the rater should be concerned with the manner of application, ie. the therapist must be articulate, comprehensible, sensitive and systematic when discussing and implementing the technique. The therapist should also be creative and resourceful in his/her selection of methods. He/she should be able to draw upon a wide range of suitable cognitive and behavioural methodologies.
It is important to remember that the same technique can have a different function depending on the stage of therapy. For example, a diary can act as an assessment tool early on in therapy, but later may serve as an effective way of promoting the re-evaluation of thought processes. The timing of the intervention is vital and must be suited to the needs of the patient. For example, if a therapist challenges basic assumptions or core beliefs too early in therapy, before he/she has a clear understanding of the patient's view of the world, the patient could feel misunderstood and alienated. Only after sufficient socialisation, should the therapist get the patient to start to reassess that level of cognition. The evaluation of automatic thoughts starts earlier, first as part of the socialisation into the cognitive model and then as change methods to improve mood and to improve on coping behaviour.
As with the application of cognitive techniques, the therapist must display skill in applying behavioural methodologies. The rationale for employing the tasks should be carefully explored, and clear learning goals established. It is important to remember that behavioural tasks play a key role with respect to the reinforcement of new learning. For example, by engaging a patient in a role-play, one can assess whether the theoretical information has been truly learned and integrated into his/her behavioural repertoire. The role-play will also allow the person to practice new skills. Behavioural tasks are also useful methodologies to employ prior to asking the patient to use the activity in a homework task. For example, it is useful to get the patient to complete monitoring sheets within the session in order to ensure the task is understood correctly. In this way the behavioural methodologies are important feedback and reinforcement activities.
It is important to note that sometimes it is inappropriate to use many methodologies within a particular session. The therapist should not be penalised in such cases, when done for appropriate reasons.
CHECKLIST: OUESTIONS FOR RATERS TO ASK THEMSELVES:
- Has the therapist ensured that the patient understands the rationale underpinning the method?
- Was the method conducted skilfully?
- Were the learning goals achieved?
- Were too many/few techniques used in the session?
- Were the techniques suitable and appropriate for the patient (ie. neither too complicated nor too demanding)?
- Was the technique consistent with the formulation?
- Were the techniques administered with skill?
- Prior to using the techniques were the learning goals clearly established?
- Where necessary, was a competent explanation of the rationale of the technique given?
- Were there valuable opportunities missed when appropriate techniques could have been administered?
- Did you hear any of the following:
- What are the benefits of thinking in this way. . . and are there any problems?
- How else could you have seen this situation? Are there alternative views?
- What would you say to your best friend?
- Have you ever had the same experience in the past and reacted differently?
- Would other people have the same opinion of you?
- What are the disadvantages of thinking that way? What are the advantages?
- Let's see whether there are events/situations/experiences that disconfirm this belief about yourself?
- Can we test this assumption in the next week? What might you try and do differently to see whether your predictions are right
Item 12 - Homework Setting
Introduction
Progress is more likely to occur when patients are able to apply the concepts learned in the therapy sessions to their lives outside; homework assignments are the bridges between therapy and the real world. The current item rates the therapist's competence in setting relevant homework tasks. The tasks should be 'custom-tailored' to the needs of the patient. They should ideally test hypotheses. incorporate new perspectives, and may encourage the patient to experiment with new behaviours outside of the session. The therapist should always explain the rationale for the prospective assignments, and elicit reactions to the homework. The homework rationale should follow on logically from the contents of the session and be consistent with the formulation.
| Key features: This aspect concerns the setting of an appropriate homework task, one with clear and precise goals. The aims should be to negotiate an appropriate task for the stage of therapy in line with the conceptualisation; to ensure the patient understands the rationale for undertaking the task; to test out ideas, try new experiences, predict and deal with potential obstacles, and experiment with new ways of responding. There are three aspects to this item:
NB: Review of homework from the previous session should be rated in Item 1 (Agenda Setting). |
Homework helps to transfer within-session learning to real-life settings. To facilitate the transfer, the homework material is usually based upon material discussed in the session.
Homework also provides a structure for helping patients gather data and test hypotheses. It also encourages autonomy rather than reliance on the therapist, and therefore plays an important role in relapse prevention. To help empower the patient, and encourage compliance, the assignments should be negotiated. It also is important to explore possible difficulties, and how these might be overcome. To mitigate against potential problems. It is often useful for the therapist to suggest that the patient visualise carrying out the assignment to identify future problems.
In addition, it is desirable to get patient's feedback regarding a specific assignment ("Does it sound useful?" "Does it seem manageable?" "Is the assignment clear?" 'What will be learned from the accomplishment/non-accomplishment of the task?"). These questions will help to determine whether the patient is both clear about the task, and understands the cognitive rationale underpinning it. It is vital that the patient is aware of the cognitive aspects of the assignment and how the results will impact on his/her interpretations. Indeed, one of the important features of homework tasks is that they bring about cognitive shift, and so they must be seen as more than just isolated behavioural assignments.
Because the setting of homework tends to occur towards the end of the session, there is sometimes a tendency to rush the process. This tendency should be avoided, as it can lead to ill-prepared and unclear tasks being set. Hence it is good practice to leave sufficient time to set the homework appropriately.
CHECKLIST: QUESTIONS FOR RATERS TO ASK THEMSELVES:
- Did the therapist adequately explain the rationale underpinning the assignment?
- Did the therapist check that the patient was confident about conducting the task correctly?
- Did the patient see the relevance of the assignment?
- Was the assignment adequately planned within the session?
- Were the obstacles to conducting the plan discussed?
- Were the learning goals established sufficiently?
- Did the therapist set the most appropriate homework task?
- Was the homework material consistent with the themes from the session?
- Was the task explained sufficiently?
- Will the patient learn something useful from engaging in this task?
- Did you hear any of the questions highlighted in Figure 12.1.
Figure 12.1: Examples of questions used when setting homework assignments
CTS-R MARKING – EXTRA NOTES
Item 1 Agenda setting and adherence
Credit for:
- Focus on aims, Summarising agenda items
- Explicit reference to agenda in session
- Time allocation – approximate (rather than too specific)
Item 2 Feedback
Credit for:
- Up to a 3 for one way feedback
- Pushing for learning points
- Eliciting feedback eg. what has been the most useful thing we have found out today?
Item 3 Collaboration
Credit for:
- Non-verbal communication ie. positioning, shared written material
Item 4 Pacing and Efficient Use of Time
Credit for:
- Evidence of pacing at client’s level
Item 5 Interpersonal Effectiveness
- Given that you think x, no wonder you feel y.
Item 6 Eliciting Appropriate Emotional Expression
- Appropriate ambience for working
- Attending to changes in affect
- Opportunity taken to acknowledge affect.
- Use of skills to ↑ and ↓ affect
Item 7 Eliciting Key Cognitions
- Rating belief in cognitions
- Linking thoughts with emotion
Item 8 Eliciting and Planning Behaviours
- Omit planning behaviours
Item 9 Guided Discovery
- Socialising or synthesising questions need to be linked to a platform of learning
Item 10 Conceptual Integration
- Extra credit for eliciting maintenance mechanisms
Item 11 Application of Change Methods
- Can include planning of a behavioural experiment for after the session i.e. homework
Reflective practice has long been recognised as a key component in skills development in professional training. Trainees will complete and submit a number of assessed pieces of reflective writing based on the application of CBT techniques to both clients in the workplace and to their own lives.
CTS-R Reflection
You will be required to submit a brief reflection with your CTS-Rs. This should be between 200 and 500 words.
You may choose to reflect on one or two themes that were of relevance to the session. We would expect you to identify the area that you are going to reflect on and then provide a reflective analysis of this area followed by a plan. Your analysis should demonstrate your ability to reflect on your practice and in particular in relation to the formulation of this client’s presentation. The analysis should provide a critical evaluation of the therapy skills that you demonstrate within the recording, drawing on relevant CBT theory, research and literature and identify areas for improvement. The following model may be help with this.
The four stage experiential learning model (Kolb 1984 and Lewin 1946) in Bennett-Levy et al. (2004 p. 19) is the most widely used model in adult education (see fig. 1).
Figure 1.Experiential learning cycle (Bennett-Levy et al., 2004)
Different terms have been used by different authors to reflect the same four stages. Plan, Experience, Observe, and Reflect.
Effective learning is said to proceed through a series of these cycles.
Experience: The experience
Observe: What happened
Reflect: Making sense of what happened by
- Relating it to previous experience and knowledge
- Searching for understanding
- Generalising, abstracting principles
- Fit with the formulation
Plan: With the new understanding, how can I take this forward?
CTS-R Reflection Guidelines:
The purpose of the reflections is to demonstrate your ability to:
- Reflect on your experience of CBT practice
- Critically analyse and make sense of that experience (informed by CBT theory and literature where appropriate)
- Extract useful learning and plan for change
You will be assessed on the following dimensions:
| Introduction of topic of reflection |
|---|
|
| Experience and observation |
|
| Critical analysis |
|
| Understanding and use of theory |
|
| Summary and implications for future practice |
|
| Structure & style: |
|
| Spelling / Grammar / Typos |
|
| References |
|
Word Count: 200 - 500
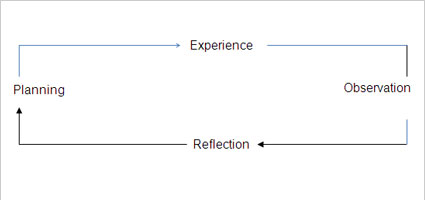
Self-Practice / Self-Reflection Tasks, Blog and Reflective Summary
Trainees will have the opportunity to engage weekly, or fortnightly, throughout the course in pre-set self-practice CBT tasks designed to prepare for or deepen learning in the concurrent taught components of the course. Trainees will be required to complete a minimum of 10 self-practice / self-reflection tasks and to write about their experience on an electronic blog on ELE which will be open to view for the current cohort and core course staff. These blogs may follow a similar format (and conform to the same 200-500 word count) to the CTS-R reflections described above but it is expected that the learning community will develop its own style.
The purpose of the blog is to encourage a community of learning in which reflective practice may be developed through the observation of and interaction with the work of others and formative feedback from experienced clinicians. Trainees will NOT be asked to post personal information on the blog but rather to reflect on the experience and insights gained that are applicable to their future CBT practice with clients. Copies of a minimum of 10 self-practice/self-reflection (SP/SR) blogs will be submitted with a reflective summary of learning for summative assessment (see guidelines and criteria for SP/SR summary below).
The self-practice/self-reflection reflective summary of learning (500 words) may follow a similar format as individual blogs and the CTS-R reflections but may cover a number of themes that have emerged from the overall experience of engaging in the self-practice/self-reflection tasks and blogs.
Bennett-Levy, J., Turner, F., Beaty, T., Smith, M., Paterson, B., & Farmer, S. (2001). The value of self-practice of cognitive therapy techniques and self-reflection in the training of cognitive therapists. Behavioural and Cognitive Psychotherapy, 29, pp. 203-220.
Self-Practice/Self-Reflection Reflective Summary Guidelines:
The purpose of the SP/SR reflective summary is to demonstrate your ability to:
- Reflect on your experience of CBT SP/SR
- Critically analyse and make sense of that experience (informed by CBT theory and literature where appropriate)
- Extract useful learning and plan for change
A minimum of 10 SP/SR blogs MUST be included as appendices to the reflective summary (the blogs are not marked but need to be included).
You will be assessed on the following dimensions:
| Introduction of topic of reflection |
|---|
|
| Experience and observation |
|
| Critical Analysis |
|
| Understanding and use of theory |
|
| Summary and implications for future practice |
|
| Structure & style: |
|
| Spelling / Grammar / Typos |
|
| References |
|
Word count:500
At the end of the course each programme member is required to submit a digital clinical portfolio which will include:
- Front sheet
- Overall Summary of supervision hours, supervised practice and 8 completed cases (a minimum of 3 different presenting problems, of which 1 of the closely-supervised should be PTSD for Cohort 12 onwards)
- Supervision contracts from each term
- Evidence of your BABCP membership
- Formative supervisors’ reports (Workplace & University)
- Summative supervisors' reports (Workplace & University)
- BABCP supervision logs (Workplace & University) evidencing a minimum of 70 hours of supervision (see calculation below)*
- Clinical log of at least 200 hours supervised CBT practice
- Client summary sheets for all 8 supervised clients (3 x closely supervised and 5 x non-closely supervised) which will include all Summative assessment feedback (case presentation and case reports), including CBT competency assessment (CTS-R & Reflection) marks for the supervised cases, a written or diagrammatic formulation, a sample of supervision preparation forms, a patient evaluation questionnaire and copies of letters/reports relating to the 8 cases.
In the clinical portfolio, the trainee and the service can be identified but no identifiable information on clients should be included. Please ensure that all identifiable information has been concealed - use of black “highlight” in a Word document is not recommended as the client detail can often be viewed by removing the highlight. It is preferable to “Export” the document to a pdf format so changes made to protect the client cannot be undone.
- CTS-R Self-rating and Reflection for 6 sessions (attach these to the client summary sheets along with the letters/reports/PEQ and supervision preparation forms) along with the markers' feedback on the 6 CTS-Rs and reflections (these should all have reached a pass/satisfactory mark)
- Teaching hours log (plus 200-500 word reflections on learning points for each taught session missed)
This clinical portfolio forms one of the required assessments for module PYCM040. It also meets the IAPT curriculum and BABCP requirements for a level 2 accredited course and will be marked as Satisfactory/Unsatisfactory.
Confidentiality Breaches in Clinical Portfolios:
- In the Clinical Portfolio, the Trainee and the Service can be identified but no identifiable client information should be included.
- In Clinical Portfolios, if confidentiality breaches occur in relation to clients, this will be marked as an automatic fail and the Trainee will be asked to address the area of concern (and any other changes) for resubmission.
Supervision
As part of the programme you will receive two hours of university-based group supervision a week. This will amount to approximately 48 actual hours of group supervision over the course year (or about 32 hours using the group formula below). You will also receive regular supervision from your workplace supervisor over the year. Combined, this will provide you with a variety of group and individual supervision, totalling a minimum of 70 hours of supervision. Over the course of the year you need to have received a minimum of 70 hours of supervision and 200 hours of supervised CBT practice.
You need to have seen at least 8 completed cases (seen for an absolute minimum of 5 sessions but usually more, from start to completion/termination) and have received 5 hours minimum of supervision, from a supervisor who is a BABCP accredited therapist, on each of these cases. The University will provide the supervision for up to 3 of these cases.
You need to have worked with a minimum of 3 different problem presentations and one of these should be Post traumatic stress disorder (PTSD).
Please note that when calculating your supervision hours for the 8 cases, it is recognised that time spent in group supervision offers greater value than simply calculating the time spent on an individual’s case, and dividing the overall time spent in the group by the number of participants.
The BABCP recommends using the following two calculations:
1: Time spent discussing a particular case in group supervision is multiplied by two.
For example, if there are three participants in a two-hour group, 30 minutes might be spent discussing each case.
30 minutes x 2 = 60 minutes’ equivalent case supervision time.
This calculation should be used for the ‘Client Summary Sheet’ and also on the ‘Overall Summary Sheet’.
2: Overall group clinical supervision equivalent time is calculated in the following way:
The time spent in the group is divided by the number of participants in the group, and this time is then doubled.
For example, if there are 3 participants in the group, and the group meets for two hours; the formula would be
2 hours divided by 3 people = 40 minutes x 2 = 80 minutes equivalent group supervision time.
*This calculation should be used for the ‘Supervision Log’.
3 of these 8 cases you bring to University supervision must be closely supervised. This means they will also have to be formally assessed using video or live practice and assessed to be to a reasonable standard as judged by the CTS-R. The recordings you submit at the end of term 2 and in term 3 will meet the ‘closely supervised’ requirement.
Supervision Reports - At the end of terms 2 and 3, both University and Workplace supervisors will complete formative supervisor’s reports. You will need to submit these at the end of terms 2 and 3 and keep a copy for your records. You must submit your supervisor reports via PDF document via Turnitin and keep a copy for your Clinical Portfolio. At the end of term 4, both University and Workplace supervisors will complete Summative supervisor’s reports. You will need to submit your Summative supervisor reports at the end of term 4 via PDF document via Turnitin and keep a copy for your records. You must also submit your Summative supervisor reports in your Clinical Portfolio. Please note that all supervisor’s reports must be hand-signed and you should keep the original copies of your reports.
Please ensure that you directly observe your CBT supervisor (or another accredited therapist) by sitting in on a live session at least once over the year.
Clinical hours
In order to achieve at least 200 hours of supervised CBT practice by the end of the course, it is recommended that trainees aim to have completed 40 clinical hours by the end of term 1 and 90 clinical hours by the end of term 2. Clinical hours will be discussed as part of 1:1 tutorials each term.
1:1 Tutorials
Each term, you will have a 1:1 tutorial. It is a requirement that you bring your developing clinical portfolio which should include:
1. Overall summary sheet
2. Clinical Log
3. Supervision Log
4. Teaching Log
5. Supervisors' Reports (University and Workplace)
6. Update on Clinical Portfolio progress
Your tutor will review these with you in your 1:1 tutorials.
Please allow some time to prepare for your tutorial using the tutorial preparation form, these documents and your tutorial questions/issues in advance of meeting with your tutor (also see HI Course Handbook).
Mitigation Requests
Application for mitigation of assessment should be made prior to the assessment deadline in question. Students are responsible for making applications for mitigation for the affected module/element of assessment.
Students can request 72 hour evidence-free extensions (coursework only) via the eBART system (see more details below). For mitigations of up to 2 weeks and longer, students need to submit a mitigation form (found on the forms page) within one working day of the assessment to cedar-mitigations@exeter.ac.uk.
Students may apply for mitigation for more than one module where the same circumstances have affected more than one assessment. However, students must use the correct mitigation form and be explicit in detailing: the circumstances that have affected them, how these circumstances have affected their performance and evidence to support their application (doctor's note etc.), together with written corroboration/support from their workplace supervisor.
Please be clear on your form which assessment you are applying for mitigation for by providing the module code (e.g. PYCM037) and the title of your assessment (e.g. Extended Case Report). If you do not provide the correct module code and title of the assessment there may be delays for processing your application.
Where we do not receive correctly completed mitigation forms and supporting evidence, the assessment will be marked as late until the correct documentation is provided by the student.
Late applications for mitigation (made after the original assessment deadline) should only be considered in exceptional circumstances, where there are compelling reasons why the application was not made at the time. Examples may include an emerging condition, the effect of which was not clear at the time of the examination/during completion of the assignment, or a condition such as severe clinical depression which affects a student’s ability to understand or engage with the procedures.
- Students can request 72 hour evidence-free extensions (coursework only) via the eBART system. Please note this is only available for submissions made via eBART and limited to 4 occasions in a 12 month period. All applications for non-BART assessments must be made via the evidence-based mitigation process below. Students with an ILP that specifically supports the possible need for extensions will have no limit to the number of eBART extensions in a 12 month period.
- To request a first evidence-based mitigation of up to 2 weeks: please submit a CEDAR mitigation form outlining the impact your circumstances are having on your ability to meet a deadline. If the request is on clinical grounds you must also submit a CEDAR Supplementary Clinical Mitigation Form (found on the forms page) from your workplace supervisor.
If you know when requesting a first mitigation that 2 weeks will not be sufficient, in exceptional circumstances, you can request an extension of up to 3 weeks. Where more than 2 weeks is needed, you can request a deferred deadline – these are set by programme teams to support students to stay on track.
- To request a mitigation on the deferred extension deadline: please submit a request form (as above) with the relevant deferred extension deadline included. If the request is on clinical grounds, you must also submit a supplementary information form (as above) from your workplace supervisor.
If you are unable to submit by the deferred extension deadline, you may be able to request a further deferred deadline. Please note that you will need to discuss a further request with your personal / module tutor before submitting a mitigation. This is to problem-solve issues, signpost support and consider options such as interruption.
- To request a THIRD/further mitigation: please submit a request form (as above) with the relevant deferred extension deadline included AND an email from your personal / module tutor confirming the request has been discussed. If the request is on clinical grounds you must also submit a supplementary information form (as above) from your workplace supervisor.
Please note there is no requirement to disclose personal circumstances to your tutor when discussing mitigation, if you do not wish to do so.
Deferred assessment deadlines for Cohort 14:
PYCM040 Case Presentation: 1st November 2021
PYCM039 Anxiety Essay: 29th November 2021
PYCM039 Anxiety Case Report: 10th January 2022
PYCM039 Competency Tape and Reflective Summary: 14th January 2022
PYCM038 Depression Essay: 25th April 2022
PYCM038 Depression Case Report: 9th May 2022
PYCM038 Competency Tape and Reflective Summary: 20th May 2022
PYCM037 SPSR Summary: 13th June 2022
PYCM040 Competency Tape and Reflective Summary: 25th June 2022
PYCM037 Extended Case Report: 4th July 2022
PYCM040 Clinical Portfolio: 5th August 2022
Late Submission of assessments
For information on late submission of assessments please refer to: http://as.exeter.ac.uk/academic-policy-standards/tqa-manual/aph/settingandsubmission/#late
Below you will find materials that you will need to refer to or use throughout the programme.
Case Reports
Case Presentation
Essays & SPSR
Resubmissions
Portfolios
- Clinical Portfolio Cover Sheet
- HI Portfolio Review Form
- Clinical Portfolio Overall Summary Sheet
- Summative University Supervisor's report
- Workplace Supervisor’s Report (Summative)
- University Supervisor’s Report (Formative)
- Workplace Supervisor’s Report (Formative)
- BABPC Supervision log
- Clinical Log
- Client Summary Sheet Closely Supervised
- Client Summary Sheet Non-Closely Supervised
- CTS-R Self Rating and Self Reflection
- Teaching Log hours
Supervision
- Supervision Contract
- Consent to recording supervision
- HI IAPT HASQ Form (H.A.S.Q)
- Supervision Preparation Form
- Supervision Preparation Template (Padesky)
- Reflective Practice Log
- University Supervisor’s Report (Formative)
- Workplace Supervisor’s Report (Formative)
- Record of Supervision
- Workplace Supervisor’s Report (Summative)
Competency Tape Forms
- Summative CTS-R Cover Sheet
- Formative CTS-R Cover Sheet
- Summative CTS-R Cover Sheet
- Formative CTS-R Cover Sheet
- CTS-R Self Rating & Self-Reflection
- CTS-R rating scale
- Consent to Record
1 to 1 Tutorials
Mitigation form
Case Reports:
- In Case Reports there should be no identifiable information in relation to the Client or Service.
- A minor breach in Case Reports, where confidentiality/anonymisation has occurred and been acknowledged by the author, but then a minor mistake(s) gets picked up will be returned to the author for correction. The Trainee will have 48 hours (excluding weekends) to reply and correct the errors, otherwise it will be marked as a fail. The Trainee will be notified via their University email account by the Programme Administrator. If the breach occurs during a vacation period, then they will also receive an alert to their work and personal email addresses (where these have been provided) asking them to urgently check their University accounts.
- When major breaches are present or anonymisation has not occurred and/or been made explicit, this will be an automatic fail and the Trainee would need to resubmit a second submission correcting the error (and making any other changes if there are any other resubmission criteria).
Clinical Portfolios:
- In the Clinical Portfolio, the Trainee and the Service can be identified but no identifiable information on Clients should be included.
- In Clinical Portfolios, if confidentiality breaches occur in relations to Clients, this will be marked as an automatic fail and the Trainee will be asked to address the area of concern (and any other changes) for resubmission.
Case Presentations:
- With Case Presentations, no identifiable information should be presented on the Client or the Service.
- A minor breach in Case Presentations, where confidentiality/anonymisation has occurred and been acknowledged by the author, but then a minor mistake(s) gets picked up will be returned to the author for correction. The Trainee will have 48 hours (excluding weekends) to reply and correct the errors in the presentation handouts, otherwise it will be marked as a fail. The Trainee will be notified via their University email account by the Programme Administrator. If the breach occurs during a vacation period, then they will also receive an alert to their work and personal email addresses (where these have been provided) asking them to urgently check their University accounts.
- When major breaches are present or anonymisation has not occurred and/or been made explicit, this will be an automatic fail and the Trainee would need to resubmit a second submission correcting the error (and making any other changes if there are any other resubmission criteria).



